Introduction
The giant cell fibroma is an interesting non neoplastic lesion of the oral mucosa. It was first described by Weathers and Callihan in 1974. [1] It was named for its characteristically large, stellate-shaped, mononuclear and multinucleated giant cells. [1] The authors examined more than 2,000 specimens in a group of fibrous hyperplasias, and 108 met their criteria for this "new" lesion which they called GCF.
Before Weathers' and Campbells' distinction of GCF, Eversole and Rovin [2] compared and contrasted 279 fibrous hyperplastic gingival lesions, which fell into four categories: pyogenic granuloma, peripheral gingival fibroma, peripheral giant cell granuloma, and peripheral ossifying fibroma. Each has its own diagnostic histopathologic characteristics but exhibit overlap of clinical presentation. Speculations from the study were that all four types of lesions are merely varied histologic responses to common etiologic factors, but similar to one another and to other fibrous hyperplasias.
Fibrous hyperplasias are considered reactive proliferations of fibroblastic tissue rather than neoplastic proliferations. Most are the result of chronic injury or irritation. GCF was at one time hypothesized to be virus-induced, but that claim was never substantiated; therefore, it is believed to arise as a result of a stimulus, source of which cannot always be determined. [3]
There is no gender predilection for GCF, but it is a lesion of the young, found most commonly in the first three decades of life. [4]
It may be pedunculated or sessile and is found most commonly on the gingiva, with the mandibular gingiva being affected more than the maxillary. It may also be found in extragingival sites, including the tongue, palate, and buccal mucosa. It is typically of normal mucosal color unless traumatized during mastication or oral hygiene procedures. [5]
Microscopic examination usually shows multiple large stellate-shaped and sometimes multinucleated fibroblasts (giant cells) in a loosely arranged vascular fibrous connective tissue. [4]
Case Report
A 38 year old male reported to the Department of Oral & maxillofacial pathology, (Vinayaka missions Sankarachariyar dental college - Salem, Tamilnadu) with a chief complaint of a small swelling on the left maxillary gingiva since 2 months. [Fig1]
 | FIG 1: Smooth exophytic growth on the maxillary gingiva in relation to 23.
 |
The patient was a known smoker since 10 years. No other relevant medical history was found, his vital signs were normal.
On clinical examination a well defined round swelling was seen measuring 1x1 cm in relation to the left maxillary canine. [Fig 2] No surface discharge was seen, the mucosa over the swelling was same as that of the normal mucosa. On palpation the inspectory findings were confirmed, the swelling was firm and non tender. It was immobile. The mouth opening was normal. Generalized extrinsic stains were seen around the cervical thirds of all the teeth.
 | FIG 2: Round and sessile growth, colour is normal as that of the adjacent mucosa.
 |
Routine blood examination was normal.
An excisional biopsy was performed under local anesthesia and the specimen was subjected to histopathological examination which revealed a dense fibrous stroma, large stellate shaped fibroblasts were seen. [Fig 3], [Fig 4] Multinucleated giant cells were also seen among the large plump and stellate shaped fibroblasts some of which are smudged. [Fig 5]
 | FIG 3: 10 X view H&E stain showing a fibrous connective tissue with few blood vessels and minimal or absent inflammatory cells.
 |
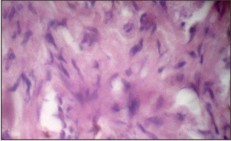 | FIG 4: 10 X view H&E stain shows large stellate shaped fibroblasts in a dense stroma, nuclei are enlarged and stellate without hyperchromatism.
 |
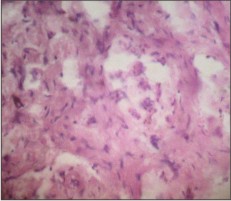 | FIG 5: Dense stroma showing stellate shaped fibroblasts and multinucleated giant cells.
 |
A final diagnosis of giant cell fibroma was established.
Discussion
The GCF was first described as a separate entity among fibrous hyperplastic soft tissue lesions by Weathers and Callihan in the early 1970s. GCF is a fibrous tumor with distinctive clinicopathology unlike traumatic fibroma; it is not associated with chronic irritation. It represents approximately 2-5% of all oral fibrous proliferations. [3]
After distinguishing GCF among fibrous hyperplasias, Weathers and Callihan further elucidated the structure of the lesion when they studied them under light microscopy. They concluded again that dominant cells in the GCF were indeed unique, and that GCF merited its own classification. [6]
The lesion usually occurs at young age of less than 30 years in about 60% of cases. Most studies show female preponderance. 50% of all cases occur on the gingiva. The mandibular gingiva is affected twice more than the maxillary counterpart. Our case has occurred in a male patient on the mandibular gingiva. Tongue and palate are next preferred sites for GCF in the oral cavity. [7]
It can be seen in other sites, especially the nose, and differs from irritation fibroma in two ways: it contains cells (fibroblasts) with large, angular nuclei, especially near the surface of the fibrous mass, beneath the overlying epithelium; and it has a greater tendency to recur.
The histologic composition of GCF is the consistent diagnostic feature of the lesion. Microscopic examination shows multiple large stellate-shaped and sometimes multinucleated fibroblasts (giant cells) in a loosely arranged vascular fibrous connective tissue. The lesion is characterized by a diffuse, somewhat immature, rather avascular collagenic stroma with small bipolar and slightly stellate fibroblasts scattered throughout in moderate numbers. Occasional fibroblasts will be quite large and angular, and may have more than one nucleus. These pathognomonic cells are never hyperchromatic, as they would be if they were truly dysplastic fibroblasts, and they often have a smudged appearance. [7]
Differential diagnosis encompasses a wide array of lesions, it differs significantly from routine fibromas in that its stroma contains scattered fibroblasts with very large, usually angular (stellate), but not hyperchromatic nuclei. The clinical diagnosis of ossifying fibroma was a logical inclusion in the differential diagnosis of this lesion, as it can look much like the GCF clinically, ossifying fibromas are typically normal mucosal color like GCFs, but they have islands of osteogenic cells dispersed throughout the lesion.
Unlike GCF, peripheral ossifying fibroma is found only in the gingiva, occurs more in females, and is thought to arise from the periodontal ligament. [8], [9]
Color and vascularity of lesions can also be distinguishing features when diagnosing fibrous hyperplasias. Most irritation fibromas are of normal mucosal color, unless traumatized, in which the lesion could appear reddened, or whitish due to hyperkeratinization, the result of continued irritation after development of the lesion. Pyogenic granuloma, on the other hand, is commonly found on the gingiva (like GCF), but tends to be red and bleeds easily if manipulated. [10]
Savage and Monsour [11] retrospectively reviewed the histologic features of all lesions designated as fibrous or fibroepithelial polyps over a 10-year period. They concluded that the histologic features were not sufficiently unusual or characteristic in normal or pathologic tissues to warrant grouping the lesions as a separate and distinct entity.
This lesion should not be confused with giant cell fibroblastoma, a term often used by general pathologist and dermatologists. This lesion is a true benign neoplasm and has a distinctive subcutaneous/dermal mass of 2-6cm seen mostly in young boys. It is not related to GCF of oral cavity. [12]
The treatment of choice for GCF is conservative surgical excision GCF seldom recurs, nor does it regress spontaneously because the excess collagen in the lesion is permanent tissue. Periodontal root planing is also suggested during excision to remove possible sources of irritation. There is no risk of transformation to cancer.
Our case is in agreement with the literature on age, pain, location, and presenting signs of the lesion.
Conclusion
Although most fibrous hyperplasias are relatively innocuous lesions, histologic examination of the tissue is necessary in most cases to rule out the possibility of malignancy. Though they are not considered true tumors, fibrous hyperplasias may continue to increase in size until the stimulus or irritation is removed or the lesion is excised. In our case the patient was a smoker hence early diagnosis was necessary to rule out malignancy.
Acknowledgements
We would like to thank Dept. of Oral Medicine & Radiology and Prof. Dr. Thiruneervannan (Principal, Vinayaka Missions Sankarachariyar Dental College) for his guidance and encouragement.
References
1. Weathers DR, Callihan MD. Giant cell fibroma. Oral Surg Oral Med Oral Pathol 1974; 37:374-84.
2. Eversole LR, Rovin S. Reactive lesions of the gingiva. J Oral Pathol. 1972; 1(1): 30-8.
3. Reibel J. Oral fibrous hyperplasias containing stellate and multinucleated cells. Scand J Dent Res. 1982; 90(3): 217-226.
4. Houston GD. The giant cell fibroma: a review of 464 cases. Oral Surg Oral Med Oral Pathol. 1982; 53(6): 582-7.
5. Rajendran R. Benign and Malignant tumors of the oral cavity. In, Rajendran R, Sivapathasundaram B (Ed). Shafer's Textbook of Oral Pathology, 6th edition. Elsevier, 2009; 127-128.
6. Weathers DR, Campbell WG. Ultra structure of the giant cell fibroma of the oral mucosa. Oral Surg Oral Med Oral Pathol. 1974; 38(4): 550-561.
7. Neville BW, Damm DD, Allen CM, Bouquot JE.Oral and maxillofacial pathology, 3rd edition, Saunders Elsevier, St. Louis, 2009, p 439-40.
8. Neville BW, Damm DD, White DK. Color atlas of clinical oral pathology. 2nd Ed. Baltimore (MD): Lippincott Williams & Wilkins; 1999. 276-7.
9. Regezi JA, Sciubba JJ, Jordan RCK. Oral pathology: clinical pathologic correlations. 4thed. St. Louis (MO): W.B. Saunders; 2003. 158-9.
10. Sapp JP, Eversole LR, Wysocki GP. Contempory oral and maxillofacial pathology. 2nd ed. St. Louis (MO): Mosby; 290-1.
11. Savage NW, Monsour PS. Oral fibrous hyperplasias and the giant cell fibroma. Aust Dent J. 1985; 30(6): 405-9.
12. Robert Marx E, Diane Stern. Oral and maxillofacial pathology: A rationale for diagnosis and treatment, 1st edition, Quintessence Publishing co, Chicago, 2003, p 396-7 |