INTRODUCTION
Although the most common cause of the intermittently suppurating cutaneous sinus tract in the face and neck area is chronic dental infection, chronic draining sinus tracts of the face and neck continue to be a diagnostic challenge (1). A review of several reported cases reveal that patients have had multiple surgical excisions, radiotherapy, multiple biopsies, and multiple antibiotic regimens, all of which have failed, with recurrence of the cutaneous sinus tract, because the primary dental aetiology was never correctly diagnosed or addressed. Few received cancer-directed therapy before having lesions correctly diagnosed (2, 3). Tidwell et al.1997 reported a case which takes over 15 years to recognize a dental origin (4). Because these lesions are often diagnosed incorrectly, they are also treated ineffectively.
This report involves a case of cutaneous facial sinus tract of dental origin, its diagnosis and treatment.
CASE REPORT
8A 22-year-old male reported to our institute complaining of sensitivity in relation to upper right posterior tooth. On examination it was found that there was carious lesion in relation to maxillary right first molar for which composite restoration was advised.
Extraoral examination also revealed erythematous, symmetrical, non tender elevated nodule (1 X 1 cm in size) with crusting and history of periodic drainage along with large skin lesion (fig 1) on right face and neck region. He stated that he had felt an induration on his cheek about one year ago and left it untreated because he had no pain.
 | Fig 1: Large Skin Lesion On Right Side Of Face And Neck
 |
However, as the lesion started to discharge pus during the following months, he then received several treatments from a dermatologist. Inspite of taking large number of antibiotics and antifungal medications both orally and topically, the lesion did not heal and the surgeon had recommended surgery now.
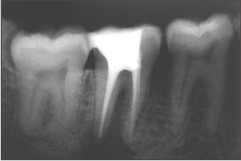
On intraoral examination, grossly carious right lower second molar was detected. The tooth was not tender to percussion or painful on biting and did not respond to electrical pulp testing. Upon radiographic examination, periradicular radiolucency in relation to carious tooth was seen. Sinus tract was tracked with a gutta-percha cone (fig 2) to the distal root lesion of the first molar tooth as seen in confirmatory radiograph (Fig 3).
 | Fig 2: Gutta Percha Passed Through Sinus Present
 |
 | Fig 3: Confirmatory Radiograph Showing Origin Of Sinus From Distal Root Of Molar
 |
Based on these findings, the patient was diagnosed as having an odontogenic cutaneous sinus tract secondary to chronic periradicular periodontitis of the left mandibular second molar tooth. His consent for endodontic treatment was taken and root canal treatment started. The skin lesion may be the result of accumulation of pus because of patient's beard leading to suprainfection. Patient was explained the dental etiology of the sinus formation and its possible management. He was even asked to get his beard shaved but patient was not wiling for that because of religious reasons.
After local anaesthesia and rubber dam placement, root canal treatment was initiated with pulp chamber access and biomechanical preparation of the root canals was done. Irrigation during instrumentation was carried out with 1% sodium hypochlorite and EDTA. Calcium hydroxide mixed with chlorhexidine paste was used as the intra canal medicament. After 1 week, lesion showed signs of healing. The canal ?lling with gutta percha and AH plus root canal sealer was performed 2 weeks after the initial appointment (fig 4) and the lesion showed further healing (fig 5).
 | Fig 4: Post Operative Radiograph
 |
 | Fig 5: Skin Lesion Showing Signs Of Healing
 |
After 1month, skin lesion healed (fig 6) and radiographic examination showed the repair of periapical tissues too. As the skin lesion have healed, patient did not turn up for further recall appointments.
 | Fig 6: Healed Skin Lesion
 |
But the present case report showed the healing of long standing cutaneous sinus and the large skin lesion (may be caused due to suprainfection from the draining pus) and thus lay stress on need of thorough knowledge about the possible dental etiology of cutaneous sinus tract in head and neck area.
DISCUSSION
A sinus tract is an abnormal channel that originates or ends in one opening. An orofacial fistula is a pathologic communication between the cutaneous surface of the face and the oral cavity. Chronic dental periapical infections or dentoalveolar abscesses cause the most common intraoral and extraoral fistulas.
As the lesion develops it is usually disregarded to be of dental origin, patient seeks treatment from a dermatologist or general surgeon and often undergoes multiple antibiotic regimens, surgical excisions, biopsies and even radiotherapy.2 Misdiagnosis adds to the chronicity of the lesion and has profound effect on facial esthetics due to unnecessary treatment resulting in cutaneoues scarring and dimpling. Only 50% of patients with cutaneous odontogenic sinus tracts have a history of toothache. Most patients are unaware of an associated dental problem (1,5), thus delaying the correct diagnosis of the cutaneous lesion with its primary odontogenic origin. One case was correctly diagnosed only after 32 years (6).
The sites of dentocutaneous fistula are usually anatomically close to the causative tooth. Of reported cases, 80% involved mandibular teeth of which half were anterior teeth, producing sinus tracts in the submental and chin sites (7). Other sites of extra-oral drainage of odontogenic origin are the cheek, canine space, nasolabial fold, nose, upper lip, and inner canthus of the eye (1,3,7).
Mandibular incisors and cuspids typically drain to the chin or submental region, and premolar and molar infections typically drain above the inferior border in the submandibular region of the anterior triangle of the neck (8). Occasionally the opening of the sinus tract may be found at a far distance from the dental infection. Endelman (9) described a patient in whom a sinus from a tooth infection opened on the chest wall and another on the upper one-third of the thigh.
Pathogenesis
Carious exposure with bacterial invasion of the tooth pulp leading to a periapical abscess is the most common cause of dentocutaneous sinus tracts. The inflammation destroys the cancellous alveolar bone and proceeds along the periosteum until perforation occurs. An intraoral or extraoral sinus can develop, depending on the path of the inflammation, which is dictated by surrounding muscular attachments and fascial planes. For example, if the bone perforation on the mandible occurs above the muscular attachment, then an intraoral sinus will result. If the perforation occurs below the level of muscular attachment, then a cutaneous sinus will result. The cutaneous lesion may develop as early as a few weeks (10) or as late as 30 years (11).
Diagnosis
Evaluation of a cutaneous sinus tract must begin with a thorough history and awareness that any cutaneous lesion of the face and neck could be of dental origin.
Dentocutaneous sinus tracts appear as soft, slightly depressed nodules, often fixed to underlying structures, with a central opening from which fluid can be expressed. Palpation of the surrounding tissue may produce pus, which supports the diagnosis.
Intraoral and dental examinations are critical for making the diagnosis. In particular, the examiner should look for dental caries or restorations and periodontal disease. Early radiographs can prevent unnecessary surgeries when the teeth appear clinically normal.A panoramic or periapical radiograph will show a radiolucency at the apex of the infected tooth.
Recognition of a sinus tract origin is the first step in diagnosis. Intraoral periapical radiographs should be taken routinely when such lesions are present, preferably with a gutta-percha cone threaded into the sinus tract. Because of gutta-percha's radiopacity, the source of the infection will be revealed. Any chronic suppurative lesion on the middle or lower portion of the face should be investigated for possible dental cause. If the primary infection site is the pulp of a tooth, the logical diagnosis would be a chronic alveolar abscess, which is defined as a long-standing low grade infection of the periradicular alveolar bone.
Biopsy, if performed, will show nonspecific findings such as pseudoepitheliomatous hyperplasia and chronic inflammation.
Most infections are polymicrobial, and culture often yields growth of anaerobes or facultative anaerobes. Sassone et al (12) performed a microbiologic evaluation of primary endodontic infections in teeth with and without sinus tract. They discovered the greatest prevalence of such bacteria as Fusobacterium nucleatum sp. vincentii, Porphyromonas gingivalis, Veillonella parvula, Enterococcus faecalis, Campylobacter gracellis, and Neisseria mucosa. The total bacterial counts were similar between lesions with and without sinus tracts, although E faecalis, Streptococcus anginosus, Capnocytophaga sputigena and Capnocytophaga gingivalis had signifcantly higher counts in those lesions without sinus tracts. Higher levels of P gingivalis and F nucleatum sp. nucleatum were noted in cases with sinus tract.
Differential Diagnosis
The differential diagnosis (1,10) should include traumatic lesions, fungal and bacterial infections, neoplasms presence of a foreign body, local skin infection (carbuncle and infected epidermoid cyst), pyogenic granuloma, chronic tuberculosis lesion, osteomyelitis, actinomycosis, and gumma of tertiary syphilis. Rare entities to be included in the differential diagnosis are developmental defects of thyroglossal duct origin or branchial cleft, salivary gland and duct ?stula, dacryocystitis, and suppurative lymphadenitis.
Treatment
Root canal therapy or surgical extraction is the treatment of choice. Root-canal therapy is done if the tooth is restorable;. Extraction is indicated for nonrestorable teeth. Once the primary odontogenic aetiology has been properly eliminated or removed, the sinus tract and cutaneous lesion usually resolve within a few weeks without treatment,
Systemic antibiotic administration is neither necessary nor recommended in patients with cutaneous odontogenic sinus tracts who have an intact immune system. Antibiotics may be used as an adjunct to sendodontic therapy in the setting of diabetes, immunosuppression, or systemic signs of infection such as fever. Antibiotic therapy alone will not be effective in these cases because of the absence of adequate circulation in a necrotic pulp system and abscess. If antibiotics are to be used, penicillin V potassium is the first choice. Clindamycin or amoxicillin-clavulanate may be used if the infection is unresponsive.
After root canal therapy, the cutaneous lesion usually resolves in 1 to 2 weeks. The patient may be left with a residual umbilication of the skin that can be surgically revised if it is cosmetically unappealing.
Conclusion:
Chronic, draining dental infection is one of the most common causes of fistulae of the face and neck. An understanding of the pathogenesis of cutaneous fistulae arising from dental infections will lead to proper early diagnosis and treatment without unnecessary surgery.
The case presented here shows that cutaneous odontogenic sinus tracts are still being misdiagnosed and that treatment applied is inappropriate. The case illustrates the need for cooperative diagnostic referrals between physicians and dentists, and highlights the need for thorough diagnostic procedures that should always include a dental examination. The clinician should recognize that a cutaneous sinus tract is a sequel to pathosis, while the associated nonvital tooth, with its periradicular periodontitis, is the primary cause.
References:
1. Cioffi GA, Terezhalmy GT, Parlette HL. Cutaneous draining sinus tract: an odontogenic etiology. Jam Acad Dematol 1986; 14: 94-100.
2. Sakimoto E & Stratigos GT. Bilateral cutaneous sinus tracts of dental etiology: report of a case. J of Oral Surg 1973; 31: 70-74.
3. Mc walter GM, Alexander JB, Delrio CE, Knott JW . Cutaneous sinus tracts of dental etiology. Oral Surg, Oral Med, Oral Path 1988; 66: 608-614.
4. Tidwell E, Jenkins JD, Ellis CD, Hutson B, Cederberg RA. Cutaneous odontogenic sinus tract to the chin: a case report. Int Endod J 1997; 30: 352-355.
5. Caliskan MK, Sen BH, Ozinel MA Treatment of extraoral sinus tracts from traumatized teeth with apical periodontitis. Endod Dent Traumatol 1995; 11: 115-120.
6. Bernick SM & Jensen JR Chronic draining extraoral ?stula of 32 years duration. J Oral Max Surg 1969; 27: 790-794.
7. Hodges TP, Cohen DA, Deck D Odontogenic sinus tracts. Americ Pract Family 1989; 40: 113-116.
8. Busselberg LF, Horton CE, Carraway JH. Cysts and sinuses of the face resulting from dental abscesses. Surg Gynecol Obstet 1979; 149: 717-718.
9. Endelman J. Dental pathology. 2nd ed. St Louis, CV Mosby, P264.
10. Spear KL, Sheridan PJ, Perry HO Sinus tracts to the chin and jaw of dental origin. Journal of the American Academy of Dermatology 1983; 8: 486-92.
11. Cohen PR & Eliezri YD Cutaneous odontogenic sinus simulating a basal cell carcinoma: case report and literature review. Plastic and Reconstructive Surgery 1990; 86: 123-7.
12. Sassone LM, Fidel R, Faveri M, Fidel S, Figueiredo L, Feres M. Microbiological evaluation of primary endodontic infections in teeth with and without sinus tract. Int Endod J. 2008; 41: 508-515. |