Introduction
Oral submucous fibrosis has been present most probably for centuries but was not described in the medical literature until 1952.1 The concept of precancers was put forward by the World Health Organization (WHO) in 1972. According to this concept, a premalignant condition is defined as "a generalized state associated with significantly increased risk of cancer". Thus by this definition the oral submucous fibrosis is classified as a premalignant condition. 2
Oral submucous fibrosis is a well-recognized potentially malignant disorder, malignant transformation rates as high as 7.6% have been reported from the Indian subcontinent over a 10-year period.3
OSMF is believed to have multi factorial cause. Numbers of factors that trigger the disease process are mainly betel nut alkaloids, ingestion of capsaicin, nutritional deficiencies, autoimmunity and genetic predisposition. However the role of betel nut chewing in one form or another remains a common denominator. Approximately 200 million people regularly chew areca nut on its own or as a part of quid, a majority of them in South East Asian countries.4
Arecanut has shown to have a higher copper content compared to the commonly eaten nuts. The copper dependent enzyme lysyl oxidase is found to be upregulated in OSMF pathway leading to increased cross-linking of collagen and elastin. Lysyl oxidase cause post-transitional modification of collagen fibers rendering them resistant to the action of collagenases.5, 6 These studies indicate that copper has a definitive role to play in the etiopathogenesis of Oral submucous fibrosis.
Aim Of The Study
The present study was under taken to evaluate the pattern of copper specific Rhodanine stain in the buccal epithelial cells of areca nut chewers, non-chewers and confirmed cases of oral submucous fibrosis and to determine its role in etiopathogenesis of Oral submucous fibrosis.
Materials & Method : This exfoliative cytological study was carried out in the Department of Oral Pathology and Microbiology.
Sample Size : For the purpose of this study, samples were distributed in three different groups.
Group A- was considered as control group i.e. Areca nut non-chewer subjects with normal oral mucosa.
Group B- Areca nut chewer subjects without clinical manifestation
Group C- Areca nut chewer Subjects having Oral Submucous Fibrosis
The samples in each group included
Group A- 10
Group B- 20
Group C- 10
Exfoliative cytology was performed for each subject using soft baby tooth brush from buccal mucosal site. Two smears were taken from each subject of a non-chewer, one smear was dipped in a copper sulphate solution for 1 hour and taken as positive control and the other smear was stained with Rhodanine to assess copper content of cells. The smears were prepared on glass slides, fixed by a commercially available alcohol based fixative and stained with Rhodanine (Lindquist method 1969) for light microscopic study.
Results
A total 40 cases were studied to analyze the presence of copper granules in buccal epithelial cells of normal oral mucosa (Group A), areca nut chewers without lesion (Group B), and OSMF patients with areca nut chewing habit (Group C) and comparison was also done between these patients in relation to duration of the habits.
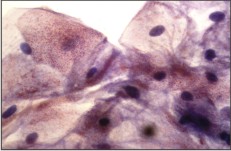
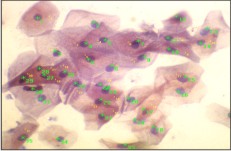
The control smears dipped in a copper sulphate solution showed pale red copper granules within the cytoplasm of all the epithelial cells. (Photomicrograph- 1, 2)
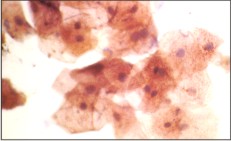 | Photomicrograph- I Smear from normal oral subjects dipped in copper sulphate solution showing copper granules taken as positive control (X40)
 |
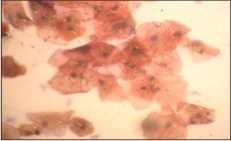 | Photomicrograph- II Smear from normal oral subjects dipped in copper sulphate solution showing copper granules counted by manual tag taken as positive control (X40)
 |
The smears of OSMF cases showed dark red stained copper granules in a large number of epithelial cells. These granules were larger and more in number and had well defined shape. The staining exhibited a granular pattern in the cytoplasm. (Photomicrograph- 3, 4)
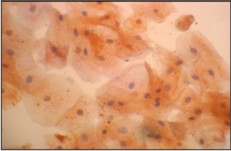 | Photomicrograph- III Smear from chewer subjects showing copper granules stained with rhodanine (X40)
 |
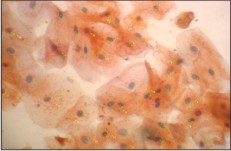 | Photomicrograph- IV Smear from chewer subjects showing copper granules stained with rhodanine counted by manual tag (X40)
 |
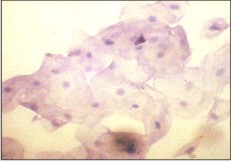
While the smears of areca nut chewers showed varying shades of pale orange red to dark red stained copper granules in a lesser number of the epithelial cells and the staining pattern was diffuse in the cytoplasm. (Photomicrograph- 5, 6)
 | Photomicrograph-V Smear from oral submucous fibrosis subjects showing copper granules stained with rhodanine (X40)
 |
 | Photomicrograph- VI Smear from oral submucous fibrosis subjects showing copper granules stained with rhodanine counted by manual tag (X40)
 |
Smears of non-chewers didn't take up any stain. (Photomicrograph- 7)
 | Photomicrograph- VII Smear from normal oral subjects taken as negative control (X40)
 |
Findings were entered in the proforma prepared for record keeping. The results were then tabulated. (Table 1) and subjected to statistical analysis using 't' test for comparing the mean score of copper granules analyzed between the groups mentioned above. The 'p' value < 0.5 was considered to be statistically significant. (Graph 1)
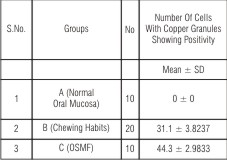 | Table I Comparison Of Cells With Copper Granules In Different Groups
 |
Then the duration of habit was compared between the chewers without lesion and OSMF patients and analyzed statistically using 'Z' test. A 5% statistically significant correlation was found. (Table 2, 3, 4)
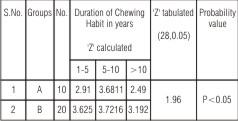 | Table 2 Comparison Of Duration Of Chewing Habit Between Group A & Group B
 |
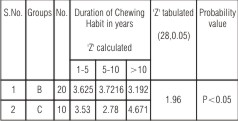 | Table 3 Comparison Of Duration Of Chewing Habit Between Group B & Group C
 |
Discussion
Recent rise in oral submucous fibrosis in globalised world, and in India particularly, has been attributed to rise in the consumption of commercially available arecanut/gutkha. Several investigators have studied the effects of the constituents of areca nut, such as arecoline and arecaidine, on oral fibroblasts in vitro in order to elucidate the etiopathogenesis of oral submucous fibrosis.7, 8 While initial studies suggested stimulation of fibroblasts in vitro by the addition of arecoline and arecaidine while others showed an inhibition.9 There has been a recent interest in the role of copper as a possible etiological factor in the development of this disorder.
In a recent study, it was reported that areca nut contains a high copper content and chewing areca nut for 5-30 minutes significantly increases soluble copper in whole mouth fluids and the copper released during chewing brought in direct contact with the oral mucosa. 10 This copper causes upregulation of lysyl oxidase in oral submucous fibrosis patients which initiates crosslinking of collagen, which makes it relatively resistant to digestion by mammalian collagenase. Therefore it is envisaged that increased lysyl oxidase activity can result in collagen accumulation. 10, 11
Earlier several studies were performed on serum copper levels in oral premalignant and malignant conditions and they revealed serum copper level to be decreased in OSMF and oral cancer (Varghese et al in 1987)12. In other study by Trivedy et al (2000) the serum samples did not display any significant alterations in OSMF subjects.13
Meghji et al (1997) had questioned the hypothesis of association of copper with OSMF on the basis that patients with OSMF have low to normal serum concentration of copper. This may be explained in several ways. Following areca nut chewing, unlike the ingestion of copper from dietary sources, effects are more likely to be local within the area of prolonged contact. Small quantities that may be absorbed by swallowing the areca containing quid will be transported to the liver by the function of copper chaperones such as Caeruloplasmin and Transcuperin. These have the buffering capacity to maintain the serum copper at a steady state, unlike in systemic disorders of copper metabolism such as Indian childhood cirrhosis or Wilson's disease in which serum copper is reported to be raised.
The above studies demonstrated that there was no increase in serum copper levels in Oral submucous fibrosis patients and studies have shown that systemic copper metabolism was not deranged. With these studies, it could be assumed that oral submucous fibrosis possibly arises due to a local abnormality of collagen metabolism rather than with a systemic basis.13
Oral submucous fibrosis is believed to be loco-lesional disease as fibrosis was evident only in the area of local contact of copper with the oral mucosa but no evidence of visceral organ fibrosis is seen (Rajendran et al 2001).14 Several factors may influence the bioavailability and subsequent absorption of copper by the oral mucosa. These factors include binding to non-soluble complexes, such as hemicellulose, dietary carbohydrates, dietary fats, the presence of amino acids, other mineral elements and the pH of the oral environment.15 This would suggest that the composition of the quid or pan masala may have a significant effect on the availability of copper in the oral cavity. The mechanism that regulate the uptake of copper by cells of the oral mucosa are also not fully understood. At a cellular level, there is evidence to support the role of membrane bound copper transporting adenosine triphosphates in the uptake of copper by cells. The exact mechanism for this is not known, but it is thought that the copper binding sites form an extended polypeptide chain at the amino terminus of the transmembrane domain.6
The reason for accumulation of copper by cells are explained by the extracellular presence of tripeptide glycyl-L-histidyl-L-lysine (GHL), where the first two residues of the GHL molecule are involved in the binding of copper, whereas the side chain of lysine may be involved in the recognition of receptors that function in the uptake of copper into cells. This tripeptide may be liberated within the lamina propria of areca chewers during the initial inflammatory phase of OSMF.16 Interleukin -1 beta which has been shown to potentiate collagen synthesis in vitro is another important regulator of fibrosis that participates in the mediation of OSMF. Any interaction of copper with other agents in the nut, such as arecoline, and mediators of inflammation, such as cytokines, need further study.6
The relative risk of chewing arecanut was assessed by comparing the duration of the habit in subjects of chewers without lesion and in oral submucous fibrosis patients. Statistical analysis was performed using 'Z' test to compare the values between the study samples.
It was found in our study that the duration of chewing was statistically significant between the groups. This is in support of a study by Sinor et al 1972 17 where it was found that both duration and frequency of chewing arecanut was directly related to the manifestation of oral submucous fibrosis. This means that exposure to total burden of various harmful substances for a long time increases the risk of OSMF.
To the best of our knowledge, till date only one study has been done to demonstrate copper in oral cytological smears of chewers and oral submucous fibrosis. (Rooban et al 2004).18
The variation in intensity, appearance and number of positive staining epithelial cells in OSMF patients could be due to changes in the permeability of the epithelium. The changes could be either due to the disease process itself i.e. atrophic epithelium or the alteration in the metallothionein that transports the copper into the cell or there is change in the spatial arrangement of copper within the cell accounting for the granular appearance in OSMF patients (Rooban et al 2004).18
Our study strongly suggests that copper in the buccal mucosal smears of OSMF patients supports the hypothesis of copper as an initiating factor in OSMF, playing a role in stimulating the fibrogenesis by the up regulation of Lysyl oxidase activity.
Conclusion
The findings of this study of orange-red stained copper granules in the cytoplasm of the epithelial cells of the Oral Sunmucous Fibrosis in oral cytological smears supports the hypothesis that transmucosal transport of copper occurs through the epithelial cells to reach the connective tissue from the saliva and play a role in the pathogenesis of Oral Sunmucous Fibrosis
References
1. Sirsat S.M., Khanolkar V.R. Submucous fibrosis of the palate and pillars of the fauces. Indian J of Medical Sciences 1962; 16 (3): 189-197.
2. Pindborg JJ. Is submucous fibrosis a precancerous condition in the oral cavity? Int Dent J 1972; 22: 474-480.
3. Murti PR, Bhonsle RB, Pindborg JJ, Daftary DK, Gupta PC, Mehta FS. Malignant transformation rate in oral submucous fibrosis over a 17-year period. Community Dent Oral Epidemiol 1985; 15: 340-1.
4. Ranganathan, K., Uma D.M., Elizabeth J, Kirankumar, K., Saraswathi, T. R. Oral submucous fibrosis: A case control study in Chennai, south India. Journal of Oral Pathology & Medicine May 2004; 33 (5): 274-277.
5. Rajendran R, Karunakaran A. Further on the causation of oral submucous fibrosis. Ind J Dent Res 2002; 13 (2): 74-81.
6. Trivedy C, Meghji S, Warnakulasuriya KA, Johnson NW, Harris M. Copper stimulates human oral fibroblasts in vitro: a role in the pathogenesis of oral submucous fibrosis. J Oral Pathol Med 2001; 30 (8): 465-470.
7. Harvey W, Scutt A, Meghji S, Canniff JP. Stimulation of human buccal mucosa fibrobalsts in vitro by betel-nut alkaloids. Arch Oral Biol 1986; 31: 45-9.
8. Jeng J.H., Lan W.H., Hahn L.J., Hsieh C.C., Kuo M.Y. Inhibition of the migration, attachment, spreading, growth and collagen synthesis of human gingival fibroblasts by arecoline, a major areca alkaloid, in vitro. J Oral Pathol Med 1996; 25: 371-5.
9. Van Wyk C.W., Olivier A, De Miranda C.M., Van der Bijl, Grobler-Rabie A.F. Observations on the effect of areca nut extracts on oral fibroblast proliferation. J Oral Pathol Med 1994; 23: 145-8.
10. Trivedy C, Baldwin D, Warnakulasuriya S, Johnson NW, Peters TJ. Copper content in Areca catechu (betel nut) products and oral submucous fibrosis. Lancet 1997; 349: 1447.
11. Rajendran R, Kumari K.R., Kumar K.S. Liver ultrasound and faecal copper estimation in oral submucous fibrosis. Ind. J dent. Res 2003; 14 (1): 13-21.
12. Varghese I, Sugathan C.K, Balasubramoniyan G, Vijayakumar T. Serum, copper and zinc levels in premalignant and malignant lesions of the oral cavity. Oncology 1987; 44: 224-227.
13. Trivedy CR, Warnakulasuriya KAAS, Peters TJ, Senkus R, Hazarey VK, Johnson NW. Raised tissue copper levels in oral submucous fibrosis. J Oral Pathol Med 2000; 29: 241-8.
14. Rajendra R, George B, Sivakaran S, Narendranathan N. Visceral organ involvement is infrequent in oral submucous fibrosis (OSF). Indian J Dent Res 2001; 12(1): 7-20.
15. Wapnir RA. Copper absorption and bioavailability. Am J Clin Nutr 1998; 67(5): 1054-60.
16. Marquart F.X, Bellon G, Chaqour B, et al. in vivo stimulation of connective tissue accumulation by the tripeptide copper complex glycyl-L-histidyl-L-lysine copper in rat experimental wounds. J Clin Invest 1993; 92: 2368-76.
17. Sinor PN, Guptha PC, Maruthi PR, Bhonsle RB, Daftary DK, Mehta FS, Pindborg JJ. A case control study of oral submucous fibrosis with special reference to etiologic role of arecanut. J Oral Pathol Med 1990; 19(2): 94-8.
18. Rooban T, Saraswathi TR, Antony George, Elizabeth George, Elizabeth Joshua, Ranganathan K. Cytological study of copper in oral sub mucous fibrosis. Ind J Dent Res 2004; 15 (4): 129-132. |