Introduction
Dentistry is both an art and a science. It is a science because our fundamental understandings - or building blocks of knowledge are founded on the scientific process of research. This includes basic, applied, and clinical research. It is an art in that it draws on experience and personal observation, because science cannot account for the complexity of all variables in each situation. The synthesis of scientific understanding and clinical observation provides the basis for meaningful dental care.1Evidence-based dentistry is an attempt to synthesize both these aspects of dentistry.
What is Evidence -Based Dentistry?
The foundation for evidence- based practice was laid by David Sackett who has defined it as "integrating individual clinical expertise with the best available external clinical evidence from systematic research".
The American Dental Association (ADA) defines evidence-based dentistry (EBD) as, "an approach to oral health care that requires the judicious integration of systematic assessments of clinically relevant scientific evidence, relating to the patient's oral and medical condition and history, with the dentist's clinical expertise and patient's treatment needs and preferences (figure-1).2
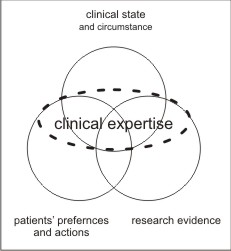 | Figure-1 : Evidence - Based Dentistry
 |
The principles of evidence-based dentistry are finding the best information quickly when it is needed, assessing its quality and deciding whether it is relevant - will help practitioner to use research evidence in making everyday clinical decisions.
Steps involved in evidence-based learning process:
Step-1: Convert the need for information about prevention, diagnosis, prognosis, therapy etc, into an answerable question which relates specifically to the patient's requirements and the population of interest.
The first step in the quest for answers to clinical questions (and often the first stumbling block) is the formulation of a clear and focused question - one that is relevant and will help to carry out a quick and effective search. Most often, the original question is too broad. The first step consists of narrowing the question by deciding which elements are the most important to answer with a "hit and run search".
It may not always be easy to formulate good clinical questions. This is especially true when dealing with situations that are not routinely familiar. In such situations, we can consider that our questions take 1 of 2 forms; those that are "background" and those that are "foreground" in nature. Background clinical knowledge would include basic knowledge such as, "what is this disorder? "What causes it? "How does it present?" Considering such background clinical knowledge, we might develop a foreground question such as "in patients with severe xerostomia, would a course of pilocarpine improve oral comfort and the quality of life (QOL) (over doing nothing) to be worth the potential side effects and cost?" Although foreground questions usually have 3 or 4 parts, background questions do not. These usually start with what, where, when, why, how and who, and end with a clinical entity, such as a health state or health intervention.4 The practitioner must decide which questions to pursue in the limited time available. The first criterion in selecting which questions to pursue is to choose questions from the patient's perspective. The second criterion suggests that practitioners seek evidence on questions that assist in staying current and in preparing for the next occasion.3
Step-2: Track down the best evidence with which to answer the question.
Several options are available, which could include asking a colleague (or expert), checking text books and their references, looking through articles in journals, or searching through a bibliographic database. But the clinician must check for quality (strength) of evidence while obtaining best possible answer to his/her question.
Quality of evidence and research design hierarchy
All clinical research studies are encompassed under the broad heading of epidemiologic studies. These studies can be further divided into- descriptive and analytical studies (observational studies) and Intervention studies or clinical trials.
A new type of studies has emerged after the advent of evidence based research i.e. integrative studies, which includes systematic reviews and meta-analysis. When the information from all relevant trials addressing the same question is combined using well-established, rigorous methodology, the result is a systematic review or overview. If the results of each trial were reported in such a way that they can be combined statistically by the researcher, the result is a quantitative systematic review or meta-analysis.
The quality of various research designs can be placed in a "research design hierarchy." The position of each research design within the hierarchy is a function of the strengths and weaknesses of features within each design. The higher the study design ranks in the research hierarchy, the better the study design minimizes bias and distributes random variation equally between the study groups. 4 The strongest evidence is replication of the study findings. Independent replications provide clear evidence that the finding is not just a random event. The researcher demonstrates that the finding is not just an artifact of a single study but a consistent event.
Next slot in the hierarchy is given to systematic review or meta-analysis. When the results of primary studies are summarized but not statistically combined, the review may be called a qualitative systematic review. A quantitative systematic review, or meta-analysis, is a systematic review that uses statistical methods to combine the results of two or more studies. By combining randomized, selected studies (or the universe of available studies) from a pool of studies meeting explicit, predetermined, experimental design criteria, the researcher can counteract and eliminate bias that occurs in each individual study reviewed.
Randomized, controlled trials represent the next highest level of evidence. This level of evidence is supported by single (nonreplicated) experimental studies in which the experimental and control conditions are clearly specified and in which assignment to the experimental and control conditions is random.
Epidemiologic surveys in which the population is sampled systematically (random, stratified sampling) and the observers are calibrated serve as the next level of evidence.
Nonrandomized studies with controls such as case controlled studies and field studies form the next level of evidence. Studies using historical controls but using randomized sampling or selection serve as the next level. Cohort studies in which disease like assignments are made using correlational analysis are next in terms of evidence. Case reports and related anecdotal or descriptive evidence are next. Finally, the reports of expert committees and the opinion of experts form the lowest level of evidence. (Figure-2)
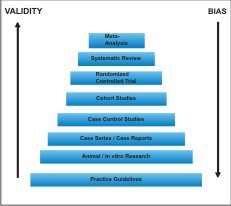 | Figure-2 : Evidence Hierarchy Pyramid
 |
Step-3: Critically appraise the evidence
Once the evidence is collected it must be screened for validity (closeness to the truth), impact (size of the effect), and applicability (usefulness in clinical practice). The user's guides are designed to test an article on these three parameters. These guides are basically a set of questions whose answers should be provided to the reader by the article in order to obtain best clinical evidence for the question in focus. A study is said to possess external validity when it can provide unbiased inferences regarding a target population (beyond the subjects of study). The impact of the evidence can be measured by the size of treatment effect for therapeutic interventions. This effect may be reported in a number of ways, depending on type of interventions.
Need for the users' guides:
When you conduct a search, how do you quickly know which article(s) to read? Are there key features to look for which can guide you to the strongest evidence? By using 3 key questions from the format of the Users' Guides, one can screen the titles and abstracts from a search to decide which are worthy of more careful study:
1. What are the results?
2. Are the results valid?
3. Will the results help me in caring for my patients?
Once these articles are identified, and if careful evaluation reveals that the results are of interest and possibly applicable to the question, then the research methods can be evaluated to determine whether they are valid or close to the truth.5
Deciding if an article is likely to provide valid results
The first question applied to any article tracked down in an effort to find an answer for a clinical problem concerns its closeness to the truth: are the results of this article valid? The Table -1 presents two key guides to assess validity for primary studies (those that provide original data on a topic) and integrative studies (those that summarize data from primary studies). For each type of integrative study, the first criterion has to do with whether the question is appropriately framed, and the second with whether the evidence was appropriately collected and summarized. The clinician can use these most important criteria to rapidly screen an abstract to determine whether it warrants the additional time required to read it in detail. These criteria can also be used to reduce the clinical literature to a manageable size when trying to keep up with new advances that are pertinent to one's practice.
 | Table - 1 Guides On Selecting Articles That Are Most Likely To Provide Valid Results
 |
Step-4:Integrate the critical appraisal with clinical expertise and with the patient's unique biology, values and circumstances.
Step-5:Finally, evaluate performance in terms of effectiveness and efficiency by questioning the ability to complete steps1-4 successfully, and seek ways to improve performance in future.
Problems And Promises With Evidence - Based Dentistry
Dental profession: in midst of lack of evidence?
With regard to dentistry, these are indeed the best of times. We have available materials and techniques that visionaries could only dream of 25 years ago. We can predictably replace missing teeth with implant-supported prosthesis. We can regenerate tissue lost to disease and trauma. And yet, as our profession entered the 21st century, these are also the worst of times. As a profession, we have become so enamoured with our new technologies that we seem to have lost our collective common sense. We have many wonderful new materials and techniques, but do we have the wisdom to use them appropriately?
The dental profession has received a great deal of criticism in the public press because of findings that enormous variations exist in treatment recommendations and health care practice. These variations have been attributed to (1) poor science underlying the clinical decisions, (2) poor quality of clinical care decisions and (3) variations in clinical skills. To counter these criticisms and to respond to the challenge of modern health care, the dentist must combine evidence-based information with practical clinical experience when engaging in the process of diagnosis, treatment planning and treatment. 7
Due to rapid flux of materials, the idea has insidiously crept into our thinking process that clinical research data is not necessary in our decision -making process. Since nature abhors a vacuum, the void created by this lack of relevant clinical research has been filled with anecdotal information. Hence, the genesis of our newest source of information, the nonrefereed dental "journal". This new class of literature is based on the premise that the refereed literature is too slow and cumbersome. It is most often written with two overriding purposes: (1) to promote a product or device and (2) to promote the career of the author.
Three factors are primarily responsible for this trend. First is the lack of an evidence-based educational philosophy in dental education. Dental schools have traditionally placed a much greater emphasis on the mechanistic aspects of dentistry. An understanding and appreciation of the dental literature as a basis for clinical decision - making has never been the primary educational focus in dental schools.
The second factor is the market forces that have created the dental infomercial. The vast majority of the nonrefereed literature is sponsored by dental manufacturers. It is packaged to simulate traditional refereed journals and is not presented as the commercial advertising it truly is.
Third and certainly the most important factor is that many of us suffer from the late 20th-century malady of busyness. With all of the activities in our personal and professional lives, it is difficult for us to maintain our commitment to reading current literature. Since time is limited and the infomercial literature is more entertaining, we read it instead of refereed journals. However, it is the dentist, not the manufacturer, who makes the treatment decisions. Therefore, the ultimate responsibility for making these decisions, based on the best available evidence, lies with the dentist.8
Barriers to using evidence-based methods
Barriers in using EBD in everyday practice include lack of appropriate skills for formulating clear questions, executing efficient electronic searches and evaluating the literature.
Often cited as a barrier to EBD is the lack of good clinical research in the form of well-designed, adequately powered randomized trials. The rigorous methodology demanded by systematic reviews for organizing and analyzing the literature in an area provides a valuable tool for identifying areas where the evidence is weak and where research is needed and feasible.
Perhaps the greatest impediments to the evidence-based movement are the fear and mistrust on the part of practitioners that the evidence will be misused by decision makers, particularly third-party funders and regulatory bodies, and that the individual autonomy of dentists, in caring for their patients, will be threatened. This is another compelling reason why the profession must embrace EBD and provide the leadership needed to protect the scientific integrity of the evidence. Practicing dentists must ensure, through direct involvement with the process, that guideline development methods are open and transparent and that the resulting guidelines are practical, useful and relevant.
Overcoming these barriers, exploiting the potential of information technology and applying sound scientific priniciples to everyday practice will allow dentists to meet the greatest challenge of practice- the provision of high quality, effective oral health care.9
Problems of introducing evidence based dentistry
1. Amount of evidence : Currently over 2 million biomedical articles are published annually in some 20,000 journals. There are about 500 journals related to dentistry. Clearly not all of these articles are relevant to all areas of dental practice, nor can one hope to read more than a small minority.
2. Quality of evidence : Much of the ever increasing volume of evidence is produced to enhance career prospects rather than to increase knowledge. This can compromise quality. A number of publications that are widely read in dentistry are not subject to peer review and even when they are there is the tendency for publication bias. This bias may not be explicit but there is a tendency both by the researchers and editors to publish positive reviews. Negative trials can be equally valuable, and concerns have been raised that increasing sponsorship of medical trials by commercial concerns could result in non-publication of negative or unhelpful findings.
3. Dissemination of evidence : Unless good methods of dissemination are available even where there is good evidence it can take many years for a particular treatment to become the norm.
4. Practice based on authority rather than evidence : The use of techniques or therapies based on the views of authority rather than evidence may lead to the wrong treatment being performed. 10
The Beginning
Dental speciality groups are now beginning specifically to address the clinical applications of evidence-based methods in clinical care. Several forums are now in place to facilitate these (r)evolutionary changes:
-
The new journals- Evidence-Based Dentistry and Evidence - Based Practice brings oral health into the fold of a burgeoning field of medical speciality journals focused on evidence-based health care.
-
Dental school curriculum are being revised to include basic information on EBD and to ensure that course content is evidence -based.
-
The Centre for Evidence-based Dentistry at Oxford University offers short-term intensive courses in Evidence-based Dentistry, a Critical Appraisal Skills Programme, and serves as the editorial centre for the journal Evidence-Based Dentistry.
-
The Harvard School of Dental Medicine's Office of Evidence-based Dentistry initiated a course "Evidence-based Dentistry" in its pre-doctoral dental curriculum, and offers a short-term, intensive graduate-level, clinical trials training program in Evidence-based Dentistry that includes an MPH degree in clinical effectiveness.11
-
The American Dental Association Commission on Accreditation requires , as part of the accreditation process of dental school curricula, that students develop the skills needed to manage scientific information will critical thinking. The requirement that students be able to locate, understand, and critically evaluate the dental literature provides some of the skill required to properly treat the patient in the clinical setting-in other words, the skill to understand, decipher, and apply evidence.1
Who will benefit from evidence- based dentistry?
In the current information era, knowledge is both a tool and a commodity that can be used to improve the decisions made by dentists every day. Information summarized within systematic reviews should assist dentists in making appropriate treatment decisions with patients. Evidence-based dentistry help dentists by providing simple and validated scientific summaries. Personal experience, because of its potential for bias, should no longer be the solel source of life long learning in dentistry. Furthermore, the lack of consistency in treatment decisions among dental and medical practices is problematic. Shifting from a reliance on the experimental model of decision making to an evidence based model would benefit all health care professions, as well as general public. 12
1. The ultimate beneficiaries of EBD are members of the public, who will reap the rewards of better care. The internet allows patients, as well as professionals, access to health care information. The public, however, does not have the tools to evaluate the data adequately and must rely on their educated dentists to help sort fact from fiction. Patients will be more educated, more involved in their treatment decisions, and more appreciative of quality care.
2. Dentists, who will also benefit from EBD. Instead of conducting free product testing for dental product manufacturers, practitioners will have at their disposal more valid research on which to predicate their clinical decisions.
Other advantages dentists may garner include: 13
-
Improved patient, staff, and dentist satisfaction.
-
Greater pride among patients, staff and dentists in high quality care.
-
Improved clinical decision making capability
-
Greater confidence in treatment planning
-
More opportunity to provide treatment choices selected for minimizing risk of harm and maximizing treatment safety
-
Greater satisfaction derived from creating customized treatment plans based on the powerful combination of stronger clinical evidence, clinical judgment and experience, as well as patient preferences and values
-
Reduced overhead and improved production by saving time and money using techniques and materials that are effective and efficient
-
Higher treatment acceptance as dentists add to their presentation tool box the sharing of high quality meaningful evidence with patients
-
Enhanced patient trust and rapport
-
Improved practice building opportunities as patients share with others their trust, confidence and pride in their EBD practicing dentist.
3. Researchers, who will benefit by being called upon to do the clinical testing necessary before new products are placed on the market.
Conclusion
Evidence-based care is a global movement in all the health sciences disciplines. It represents a philosophical shift in the approach to practice - a shift that emphasizes evidence over opinion and, at the same time, judgment over blind adherence to rules. This approach provides a bridge between research and everyday patient care. In near term future for evidence -based practice is likely to be characterized by continuation of current trends in dissemination of evidence-based information to clinicians. The primary means for dissemination will consists of evidence summaries and evidence- based treatment recommendations and guidelines.
References
1. Cruz M. Dental education,dental practice and the use of evidence. J Evid Base Dent Pract 2001;1:81- 2.
2. Goldstein GR. What is Evidence Based Dentistry? Dent Clin N Am 2002; 46: 1-9
3. Sutherland SE. Evidence-based Dentistry:Part 1. Getting started. J Can Dent Assoc 2001;67:204-6
4. Anderson JD. The Question. Dent Clin N Am 2002; 46:11-19
5. Jacob RF, Carr AB. Hierarchy of research design used to categorize the "strength of evidence" in answering clinical dental questions. J Prosthet Dent 2000; 83:137-52
6. Oxman AD, Sackett DL, Guyatt GH. Users' guides to the medical literature I. How to get started. JAMA 1993; 270: 2093-5
7. Afes VB, Hittelman E. Accessing and reading dental public health research: Evidence- based dental practice. In: Jong AW editor. Community Dental Health. 5th edition. Mumbai: Varghese publishing house; 2003. p. 391-421
8. Robbins JW. Evidence- based dentistry: what is it, and what does it have to do with practice? Anecdote vs. Data - a case for evidence- based decision making. Quintessence Int 1998; 29:796-9
9. Sutherland SE.The building blocks of evidence-based dentistry. J Can Dent Assoc 2000; 66: 241-4
10. Richards D, Lawrence A. Evidence based dentistry. Br Dent J 1995; 179: 270-3
11. Niederman R, Badovinac R. Tradition-based dental care and Evidence-based dental care. J Dent Res 1999; 78: 1288-91
12. Ismail AI, Bader JD. Evidence- based dentistry in clinical practice. J Am Dent Assoc 2004; 135: 78-83
13. Gillete J, Joseph DM, Frantsve-Hawley J, Weyant RJ. Evidence Based Dentistry. Dental Clin N Am Jan 2009;53 (1): 33-45 |