INTRODUCTION
The term temporomandibular disorder (TMD) is defined as “collective term embracing a number of clinical problems that involve the masticatory musculature, the temporomandibular joint and associated structures, or both. Temporomandibular disorders are considered to be a sub-classification of musculoskeletal disorders and are a major source of orofacial pain of non-dental origin 1.
The mandibular condyle sits in the glenoid fossa of the temporal bone forming the temporomandibular joint. Ideally the condyle should be positioned centered in the fossa about 1.5 mm from the articular eminence, 2.5 mm below the roof of the articular fossa and around 7.5 mm from the center of external auditory meatus 2. It has been proposed that the signs and symptoms of temporomandibular disorders are due to the change in the position of the condyle in the glenoid fossa 3. Some studies dispute the role of condylar position in the pathogenesis of
temporomandibular disorders due to the fact that there is a large variation in the position of the condyle in patients with temporomandibular disorders 4. Guiding the condyle into centric position in the glenoid fossa has given positive results in the management of signs and symptoms associated with TMD 5
The present study compared the position of the condyle in subjects with signs and symptoms of TMD with that of asymptomatic subjects.
MATERIAL AND METHODS
106 subjects of Bangalore of Indian origin aged between 18-48 years were selected for the study. The subjects were divided into divided into 2 groups, asymptomatic subjects (group I) and subjects with signs and symptoms of temporomandibular disorders (group II). The sample consisted of patients with normal occlusion, malocclusion or those requiring orthodontic treatment. Patients presenting with developmental abnormalities of the temporomandibular joints, subjects below 18 years of age and pregnant women were excluded from the study.
All the subjects were selected from the out patient department of Oral Medicine and Radiology. After explaining the need for study their consent was obtained on a consent form. A detailed case history and clinical examination was performed on the subjects by using a case history format.
Based on the history and clinical findings, individuals were categorized as normal subjects or subjects with the disc displacement with reduction and subjects with disc displacement without reduction. Disc displacement with reduction was diagnosed when there was clicking on both vertical opening and closing that occurs at a point at least 5mm (interincisal opeing) greater than on closing, is eliminated on protrusive opening , and is reproducible in two of three consecutive trails or click on opening or closing and click on lateral excursion or protrusion, reproducible in two of three consecutive trials.6 Disc displacement without reduction was diagnosed when there was history of significant limitation of opening, maximum unassisted opening lesser than or equal to 35mm,
passive stretch increases opening by lesser than or equal to 4mm, and contralateral excursion lesser than 7mm and/or uncorrected deviation to the ipsilateral side on opening and absence of joint sounds or sounds that do not meet criteria for disk displacement with reduction. 6
METHODOLOGY
For the study a lateral tomogram of the TMJ in both open and closed positions were taken on GENDEX Orthoralix 9200 panoramic machine. Two sets of readings were recorded at an interval of one week for the lateral tomogram. The mean of both the readings were recorded. Both right and left TMJ regions were traced on tomograms of all the subjects.
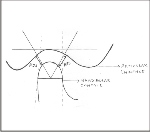
A baseline was drawn on the tracing paper by connecting the highest point of the post glenoid process to the crest of the articular eminence. A tangent was drawn to the articular fossa. A perpendicular line was drawn from the highest point on the articular fossa to the base line From this point again a perpendicular line was drawn from the tip of the post glenoid process height to the tangent drawn to the curve of the articular fossa. Another perpendicular line was drawn from the crest of the articular eminence to the tangent drawn to the curve of the articular fossa. Two lines at 60 degrees angle each–running anteriorly and posteriorly - were drawn from the point of intersection of the perpendicular line from the greatest curvature of articular fossa and the baseline.
With these demarcations anterior joint space (ajs) -smallest distance between anterior surface of condyle and fossa and posterior joint space (pjs) - smallest distance between posterior condyle and fossa, measurements were made (Figure 1).
The condylar position index (CPI) was calculated which indicated in percent an anteriorly positioned condyle when the value was positive and a posteriorly positioned condyle when the value was negative. CPI was calculated using the following formula: CPI = 100 ×(pjs – ajs)/(pjs + ajs).
Results
In subjects with DDWR, the mean of CPI was -7.817 with a standard deviation (SD) of ±20.26 and range of -60.0 – 33.33. In subjects with DDWoR, the mean of CPI was -3.465 with a standard deviation (SD) of ±12.03 and range of -20.0 - 11.11. In subjects under group I, the mean CPI was -5.91 with a SD of ±18.56 and range of -60.0 – 33.33. In subjects under group II, the mean CPI was 1.83 with a SD of ±5.33 and range of -5.88 – 33.33. The CPI value between the group I subjects and group II subjects was statistically significant (p=0. 003) (Table 1)
In group II, out of 56 subjects, 20 subjects (35.71%) had a positive CPI value indicating an anteriorly positioned condyle; 08 subjects (14.28%) had a negative CPI value indicating a posteriorly positioned condyle and 28 subjects (50.0%) had CPI value as zero indicating a concentrically placed condyle. The correlation between the anteiorly placed condyle, posteriorly placed condyle and concentrically placed condyle between the DDWR, DDWoR and normal subjects was statistically significant ( p= < 0.001)(Table2).
Discussion
Condyle position index (CPI) indicates whether the condyle is concentric, anterior or posteriorly positioned in the articular fossa. In the present study 29 out of 50 subjects who showed signs and symptoms of TMD had a negative CPI value indicating a posteriorly positioned condyle, 14 subjects had a positive CPI value indicating anteriorly positioned condyle and 7 subjects had a CPI value of 0 indicating a concentrically placed condyle. Out of 56 normal subjects, 28 subjects had a CPI value of 0, 20 subjects had a positive CPI value and 8 subjects had a negative CPI value. Based on the CPI values of the study it could be stated that majority of the normal condyles were placed concentrically or anteriorly in the fossa where as majority of the condyles in subjects with TMD were placed posteriorly in the fossa.
Condylar position is significantly associated with disc displacement, especially in joints with reducible disc displacement. The condyle tends to be dislocated posteriorly in these joints as compared with those with normal subjects. It has been suggested that the condyle may shift posteriorly in the early stages of the internal derangement 7. TMJs diagnosed with anterior disc displacement without reduction may have a posterioly placed condyle when compared to normal subjects 8.
In the study on subjective evaluation of condylar position on tomograms with arthrographic interpretation of disc position, showed that without tomographic evidence of degenerative joint disease, a statistically significant 88% to 90% of the TMJs with anterior disc displacement had condyles that were retropositioned in the fossa. Forty-two percent of the TMJs with normal disc position had posterior displacement of the condyle 9.
The occlusal pressure transmitted into the joint compartments makes the condyle slide posteriorly whereas the articular disc may be deformed and displaced from its normal position. 1.
The condylar retrusion may be secondary to altered disc position or a result of increased condylar and eminence remodeling. It may also be attributed to the rotation of the condyle posteriorly in the fossa, secondary to a fulcrum effect at the second molar, with loss of the posterior band of the disc from the height of the mandibular fossa and potential shortening of the mandibular ramus characteristic of these patients 10.
It is hypothesized that condyle position is a predictor of derangement, but mostly as an interaction with fossa shape. In the case of posterior position, a small initial forward translation movement of the condyle occurs in protrusion, equiv-alent to an auxiliary movement, until the rotational influence of the articular eminence slope is reached. This may lead to disc and disc attachment distortion and laxity in susceptible individuals and to frictional movements. On jaw closure, the nonworking side is initially more loaded and follows the most superior translation pathway, while a degree of distortion and laxity of the condyle is seen on working side until the load is transferred to the dentition in intercuspal occlusion. This may lead to the posterior positioning of the condyle, thereby propagating disk and disk attachment changes in susceptible individuals 11.
The quantitative nature of the CPI allows a definitive comparison of condyle position, even when actual differences between joints might be very small. A calculated CPI of -2, for example, would denote a less protruded condyle than would -1, though such a difference would not be appreciated subjectively.
Gross condyle position differences can, of course, be detected subjectively by experienced clinicians. However, subtle changes in condyle position will continue to remain beyond the discriminatory capabilities of even the most astute clinician or radiologist. In addition, quantification of condyle position data will probably be critical in understanding the relationships between the osseous and soft tissue components of the TMJ. These reasons form the rationale for the continued development of the TMJ measurement method described and for further evaluation of its usefulness 12.
CONCLUSION
The quantitative value of the condyle position has considerable potential usefulness because it will permit differentiations to be made between condyle positions, whether in different TMJs or in the same TMJ over an interval of time, even when the changes are so slight as to be un-observable to the human eye or on a radiograph. This may help the clinician in observing the progress of the TM joint pathology and also the efficacy of management strategies employed to treat the TMD.
 | Fig 1
 |
Figure 1: Schematic diagram showing the measurement of condylar position index (CPI)
Table 1: Condyle Position Index (CPI) between study group and control group
Table 2: Condylar Position Index (CPI)=( PJS-AJS/PJS+AJS) X 100.
CPI positive value= anteriorly placed condyle
CPI negetive value = posteiorly placed condyle
CPI = 0 concentrically placed condyle
χ2=25.77
d.f=4 p value=<0.001.
References:
1. Pereira LJ, Gaviao MBD. Tomographic evaluation of TMJ in adolescents with temporomandibular disorders. Braz Oral Res 2004; 18(3): p 208-214.
2. Baskan S, Zengýngul A. Temporomandibular joint, disorders and approaches. Biotechnol. & Biotechnol. Eq 2006; 20(2): p154-159.
3. Weinberg LA, Chastain JK. New TMJ clinical data and the implication on diagnosis and treatment. J Am Dent Assoc 1990;120:305-11.
4. Katzberg RW, Keith DA, Ten Lick WR, Guralnick WC. Internal derangements of the temporomandibular joint: an assessment of condylar position in centric occlusion. J Prosthet Dent 1983;49:250-4.
5. Weinberg LA. Definitive prosthodontic therapy for TMJ patients: Part I. anterior and posterior condyle displacement. J Prosthet Dent 1983;50:544-57.
6. Blasberg B, Greenberg MS. Temporomandibular disorders. In: Greenberg MS Glick M, Editors. Burket’s Oral Medicine- Diagnosis and Treatment. 10th ed. Ontario, Canada: BC Decker Inc; 2003. p. 271-306.
7. Kurita H, Ohtsuka A, Kobayashi H, Kurashina K. A study of the relationship between the position of the condylar head and displacement of the temporomandibular joint disk. Dentomaxillofac Radol 2001; 30: p 162-165.
8. Ren YF, Isberg A, Westesson PL. Condyle position in the temporomandibular joint Comparison between asymptomatic volunteers with normal disk position and patients with disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;80 : p 101-107.
9. Brand JW, Whinery JG, Anderson QN, Keenan KM. The effects of temporomandibular joint ID and degenerative joint disease on tomographic and arthrotomographic images. Oral Surg Oral Med Oral Pathol 1989;67: p 220-223.
10. Kinniburg RD, major PW, Nebbe B, Glover KE. Osseous Morphology and Spatial Relationships of the Temporomandibular Joint: Comparisons of Normal and Anterior Disc Positions. Angle Orthod 2000; 70: p 70–80.
11. Pullinger AG, Seligman DA. Multifactorial comparison between disk displacement with and without reduction according to tempormandibular joint hard tissue anatomic relationships in women. J Prosthet Dent 2001;86: p 407-419.
12. Blaschke DD, Blaschke TJ. A Method for Quantitatively Determining Temporomandibular Joint Bony Relationships. J Dent Res 1981; (60)1:35-43. |