INTRODUCTION
The demand for aesthetic and functional restorations has been simplified by the development of resin-based composites. The potential for greater application of resins came about with the introduction of the Bisphenol A glycidyl methacrylate, or Bis-GMA, by R.L. Bowen in the early 1960s. While the Bis-GMA formulations developed by Bowen were a major move in the right direction, the effort fell short of clinical success. 1 Since their arrival in dentistry, its chemical structure has changed dramatically, to overcome the problem of shrinkage, thermal expansion, and low strength. Inorganic filler size is the critical area that can be manipulated to improve its properties. The early generation of composites proved to be failure for posterior restorations due to their poor wear resistance, rough surface and high rate of polymerization shrinkage. This was due to large particles size of fillers. In 1970's , microfilled composites composed of colloidal silica, with small particle size fillers 0.04 μm were developed to improve wear resistance and produce a lustrous surface. However, they could not attain higher degree of filler loading which lead to expansion of resin matrix. Therefore they have poor mechanical properties and are avoided in high stress areas. Till now, the market is mainly dominated by hybrid composites since their arrival in 1980's. Hybrid composites were developed by combining glass particles with fillers of various sizes (aluminosilicates, quartz or barium aluminosilicate silica glasses) to provide better strength and smooth finish. 2
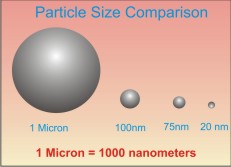
Several improvements are still going on to produce materials of adequate clinical success . Continued effort in reducing the size of fillers to improve properties has led to development of dental composites based on nanotechnology. Nanotechnology also known as molecular engineering is the production of functional materials and structures in the range of 0.1 to 100 nanometers by various physical and chemical methods. A nanomer is 1/1,000,000,000 (one-billionth) of a meter or 1/1000 of a micron ( fig:1).
 |
 |
The newly available nanomaterials are nanocomposites and nanohybrids. Nanocomposites use nanometer-sized particles throughout the resin matrix, whereas nanohybrids take the approach of combining nanometer-sized particles with more conventional filler technology. Both approaches can provide good composite materials, but the nanohybrid approach still may suffer from the loss of larger particles and the potential loss of initial gloss.3
Nanocomposite restorative materials have excellent aesthetics, polishability and very low degree of polymerization shrinkage. The development of the nanofilled composite restorative materials that have enhanced aesthetic features of high translucency and lustre still maintaining strength and wear resistance provides clinicians a reliable option for anterior and posterior restorations.4
Nanotechnology in composites
To effectively know the use and rationale of a specific composite resin system it requires an overview of the system's infrastructure. The infrastructure of composite resins consists of three basic phases - the organic phase (matrix), the dispersed phase (filler) and the interfacial phase (coupling agent).5 The organic phase or matrix of this composite resin system consists of blend of monomers that include Bis-GMA (Bisphenol-A-glycidyl methacrylate), UDMA (Urethane dimethacrylate), and Bis-EMA (Bisphenal-A-polyethylene glycol diether dimethacrylate). TEGDMA (Triethylene glycol dimethacrylate) is added to control viscosity. Matrix components also include an initiator (e. g, benzoyl peroxide for chemical activation or camphoroquinone for visible light activation), polymerization inhibitors (to extend working time and storage stability), opacifiers, and various pigments. 6,7,8 The dispersed phase or the filler particles provide strength and reinforcement to the matrix. 9,10 Currently nanofillers, the smallest filler particles are widely used in dentistry. The adoption of small nanoparticle fillers technology has noticeably improved many of the properties of composite resins. Nanoparticles are available in two forms: a single nanomer particles and a group of nanoparticles (nanocluster). 4
The nanomer particles are individual filler particles mainly spheroidal in shape. The size of nanomer-sized filler is 5-75nm as compared to the size of approx. 1 micron for conventional fillers. Nanoclusters are loosely agglomerated collections of these nanoparticles and size of approx. 2-20nm (fig:2).
The introduction of these nanosized particles allows for an increased filler loading that ultimately provide improved clinical performance through increased polishability, increased wear resistance, reduced polymerization shrinkage, and increased fracture resistance. As the particle concentration depends on the viscosity, the filler loading that can be attained 69% by volume and 84% by weight, results in reduced polymerization shrinkage and shrinkage stress. The interfacial phase or coupling agent consists of a bifunctional coupling agent that can connect the resin matrix and the inorganic filler. The most commonly used coupling agents are organosilanes.
The particle size and quantity are two crucial factors when determining how to best utilize the restorative materials. Alteration of the filler component remains the most significant development in the evolution of composite resins, because the filler particle size, distribution, and the quantity incorporated dramatically influence the mechanical properties and clinical success of composite resins. In general, the mechanical and physical properties of composites improve in relation to the amount of filler added. Many of the mechanical properties depend on this filler phase, including compression strength and/or hardness, flexural strength, elastic modulus, coefficient of thermal expansion, water absorption, and wear resistance.
Nanotechnology manufacture composite resin with nanofiller particles that are quiet small, can be dissolved in higher concentrations, and are polymerized into the resin system with molecules designed to be compatible when coupled with a polymer, and provide unique characteristics (physical, mechanical, and optical). 11 Adhesion of restorative biomaterials to the mineralized hard tissues of the tooth is a controlling factor for improving the marginal adaptation and seal, in addition enhancing the longevity and reliability of the adhesive restorations. The particle size of conventional composites are very dissimilar to the structural sizes of the hydroxyapatite crystal, dentinal tubule, and enamel rods, that there is a potential for loss of adhesion between the macroscopic (40 nm to 0.7 nm) restorative material and the nanoscopic (1nm to 10 nm in size) tooth structure. 12 Nanocomposite resin system has the ability to improve this continuity between the tooth structure and the nanosized filler particle to provide a good marginal seal between the mineralized hard tissues of the tooth and these improved restorative biomaterials.
Manufacturing approach with bottom-up approach
Nanotechnology has reintroduced the focus on manufacturing newer and smaller materials. Traditional manufacture of filler particles for dental composites has required the comminution of larger particles of quartz, glass, or ceramics through grinding or milling to small particle size. But this process can not reduce the filler particle size below 100 nm (1 nm=1/1000 µm) in diameter. To overcome this problem, direct molecular assembly, or "bottom-up" processes that involve synthetic chemical processes is used. It is the assembly of these materials into progressively larger structures and then transform them into nanosized fillers suitable for a dental composite. 4
DISCUSSION
Providing laudable advantages of tooth structure conservation, improved biomechanical properties and metal-free alternative, direct composite resin restorations are now routinely used in restorative dentistry. 13 Composite resins were first recommended for use in posterior teeth restoration more than two decades ago. While the early formulations were characterized by numerous problems, the most significant were polymerization shrinkage, marginal adaptation, inappropriate proximal contact and secondary caries still persist for many practitioners.
Recently, a new concept based on nanofillers in composite resin has developed. Due to improvement in both esthetic and physicomechanical properties, nanocomposites are becoming the popular esthetic and durable restorative materials in clinical practice. In addition it has directed the clinician's attention toward more conservative and non-invasive treatments. 14 Nanocomposites, where nanosized reinforcements (fillers) are dispersed in the base material (matrix), offer a novel class of composites with superior properties and added functionalities. The color change in a composite restorative material may be easily related to the nature of its resin matrix. The presence of low TEGDMA content in nanocomposites may its limit water uptake and, consequently, less staining. Filler particle size and distribution have been also shown to play an important role in this context. 15 Some studies have reported high surface roughness of composites, even after finishing and polishing, due to irregularly arranged inorganic filler particles, which could result in easier staining over time. 16,17Surface gloss is another factor playing an important role on the appearance of tooth-coloured restorative resins.18 Proper finishing and polishing should establish a smooth, glossy surface texture with optimum restoration contour facilitating the removal of plaque. 19-21 Especially restorations in close contact to gingival tissues require surface smoothness for optimal gingival health. The size and composition of the filler particles of the restoratives determine the material's ability to be finished and polished, thus the smoothness of the restoration. 22
Another phenomenon that contributes to aesthetic restorations is the translucency of disperse nanoparticles. Since the particles are smaller than wavelength of visible light, absorption does not occur and light shines through it. There is also greater scattering of light with the small sized nanoparticles as compared to a larger-particle composite. More scattering of light produces excellent blending of the restoration (the “Chameleon effect”) and gives it a life-like effect. In addition, the resins made with this type of small particles give the restoration a better finish, which is observed in its surface texture, and the likelihood of the material's biodegrading over time is reduced. This technology has also achieved sufficiently competent mechanical properties for the resin to be indicated for use in the anterior and posterior segments thus making them “universal” composites. It should also be mentioned that the lower size of the particles leads to less curing shrinkage, creates less cusp wall deflection and reduces the presence of microfissures in the enamel edges, which are responsible for marginal leakage, colour changes, bacterial penetration and possible post-operative sensitivity. 23,24
Under controlled wear conditions, it was found that nanocluters are formed by fusing or sintering these nanometer-sized particles and only very small, individual nanometer-sized particles can break from the clusters. The nanoclusters are designed to fracture only during wear conditions, rather than be plucked out. Thus, a smoother finish and higher gloss is retained. In comparison, a hybrid is comprised of large, micron-sized particles that, when plucked out or broken off, leave voids that significantly reduce initial polish. The initial gloss of these hybrids can be very impressive clinically. But with time and wear, individual particles of conventional hybrids are plucked from the resin matrix resulting in a reduction of gloss on the surface. It is suggested that the long-term polishing retention arises from the exposed nanoparticle fillers in the resin matrix during wear, tooth brushing, or polishing. These fillers may act as a nano-polishing medium on the surface of the composite providing long-term retention of gloss. 25 These nanocomposite restoratives have also proven to have the strength comparable to a hybrid. This is because of its high-filler loading and advanced resin matrix that result in improved strength measurements like compressive, flexural, diametral strength and fracture toughness needed for posterior restorations. It was also shown that different formulations of nanocomposites display similar or even better results regarding compressive strength and fracture toughness than conventional composite materials. 26
The polymerization shrinkage in composite resin is reported to be 1.4% to 1.6%. The low shrinkage value of nanocomposites is due to the low shrinkage epoxy resin and strong interfacial interactions between resin and nanoparticles.
As the interparticle dimension in nanocomposite decreases, the loadbearing stress on the resin is reduced, inhibiting crack formation and propogation. The spheroidal shape of the nanofillers provides smooth and rounded edges, distributing stress more uniformly throughout the composite resin. This phenomenon has been termed the “roller bearing” effect, and is said to improve the sculptability and handling characteristics.
Recently, nanoparticles of calcium phosphates were synthesized and incorporated into dental resins. 27,28,29 The high surface area of the nanoparticles, coupled with strong reinforcement fillers, resulted in composites with stress-bearing and Ca and PO4 releasing capabilities. Its strength was 2-3 times higher than previously-known Ca-PO4 composites and resin-modified glass ionomer. This composite may have the potential to provide the necessary combination of load-bearing and caries-inhibiting capabilities. 30
CONCLUSION
Nowadays, composites have unquestionably acquired a prominent place among the restorative materials employed in direct techniques. The recent integration of nanoparticles represents the continued research in the profession toward the ideal composite material. Earlier it was often difficult to achieve aesthetics as well as mechanical stability with resin- based composites. Adding nanoparticles into dental composite has imparted extraordinary physical properties, in reference to strength and durability, long term polish retention and high surface gloss beyond what current restorative materials offer. In the ending note it can be concluded, that the long standing wait for a universal restorative material in dental application may be considered over with the advent of nanocomposites.
REFERENCES
1. Leinfelder KF. New developments in resin restorative systems. J Am Dent Assoc 1997;128:573-581.
2. Yoonis E.,Kukletova M. Tooth-colored dental restorative materials in primary dentition. Scripta Medica.2009;82(2).
3. Swift Jr. EJ. Composites. J Esthet Restor Dent. 2005;17(1):3-4.
4. Mitra SB, Wu D, Holmes BN. An application of nanotechnology in advanced dental materials. J Am Dent Assoc. 2003;134(10):1382-1390.
5. Talib R. Dental composites: A review. J Nihon Univ Sch Dent. 1993;35(3).
6. Ruvter IE. Composites-Characterization of composite filling materials: Reactor response. Adv Dent Res. 1988;2(1):122-129.
7. Ferracane JL. Current trends in dental composites. Critical Reviews in Oral Biology Medicine. 1995;6(4):302-318.
8. Chung KH, Greener EH. Correlation between degree of conversion, filler concentration and mechanical properties of posterior composite resins. J Oral Rehabil. 1990;17:487-494.
9. Ehrnford L. Dental composites reinforced with microporous sintered glassfiber networks. Swed Dent J. 1983;7(suppl 18):1-34.
10. Lutz F, Sectos JC, Phillips RW, Roulet JF. Dental restorative resins: Types and characteristics. Dent Clin North Am. 1983;27(4):699-712.
11. Leinfelder KF. Composite resins: properties and clinical performance. In:O'Brien WJ, Powers JM, eds. Dental Materials: Properties and Selection. Quintessence Publishing; Chicago, IL:139-157.
12. Muselmann M. Composites make large difference in "small" medical, dental applications. Comp Tech. 2003:24-27
.
13. Ali Riza CETIN and Nimet UNLU. One year clinical evaluation of direct nanofilled and indirect composite restorations in posterior teeth. Dental Materials Journal. 2009;28(5):620-626.
14. Fontes ST, Fernandez MR, Moura CM, Meireles SS. Color stability of a nanofilled composite: Effect of different immersion media. J Appl Oral Sci. 2009;17(5):388-391.
15. Rodrigues SA Jr, Scherrer SS, Ferracane JL, Della Bona A. Microstructural characterization and fracture behaviour of a microhybrid and a nanofill composite. Dent Mater. 2008;24(9):1281-1288.
16. Guler AU, Kurt S, Kulunk T. Effects of various finishing procedures on the staining of provisional restorative materials. J Prosthet Dent. 2005;93(5):453-458.
17. Patel SB, Gordan VV, Barrett AA, Shen C. The effect of surface finishing and storage solutions on the color stability of resin-based composites. J Am Dent Assoc. 20004;135(5):587-594.
18. O'Brien WJ, Johnston WM, Fanian F, Lambert S. The surface roughness and gloss of composites. J Dent Res. 1984;63:685-688.
19. Stanford WB, Fan PL, Wozniak WT, Stanford JW. Effect of finishing on color and gloss of composites with different fillers. J Am Dent Assoc. 1985;110:211-213.
20. Inokoshi S, Burrow MF, Kataumi M, Yamada T, Takatsu T. Opacity and color changes of tooth-colored restorative materials. Oper Dent. 1996;21:73-80.
21. Turkun LS, Turkun M. The effect of one-step polishing system on the surface roughness of three esthetic resin composite materials. Oper Dent. 2004;29:203-211.
22. Roeder LB, Tate WH, Powers JM. Effect of finishing and polishing procedures on the surface roughness of packable composites. Oper Dent. 2000;25:534-543.
23. Geraldi S, Perdigao J. Microleakage of a New Restorative System in Posterior Teeth. J Dent Res. 2003;81:1276.
24. Meyer GR, Ernst CP, Willershausen B. Determination of Polymeriza-tion Stress of Conventional and New "Clustered" Microfill-Composites in Comparison with Hybrid Composites. J Dent Res 2003;81:921.
25. Terry DA . Direct application of a nanocomposite resin system: Part 1-The evolution of contemporary composite materials. Pract Proced Aesthet Dent. 2004;16(6):A-X.
26. 3M-ESPETM Supreme Plus Universal Restorative System technical product profile. 2008.
27. Xu HHK, Sun L, Weir MD, Antonucci JM, Takagi S, Chow LC. Nano dicalcium phosphate anhydrous-whisker composites with high strength and Ca and PO4 release. J Dent Res. 2006;85:722-727.
28. Xu HHK, Weir MD, Sun L, Takagi S, Chow LC. Effect of calcium phosphate nanoparticles on Ca and PO4 composites. J Dent Res. 2007;86:378-383.
29. Xu HHK, Weir, Sun L. Dental Nanocomposites with Ca-PO4:Effects of reinforcement, dicalcium phosphate particle size and silanization. Dent Mater. 2007;23:1482-1491.
30. Xu HHK, Weir MD. Calcium and phosphate ion releasing composite: Effect of pH on release and mechanical properties. Dent Mater. 2009;25(4):535-542.
|