|
|
|
| Recurrent Odontogenic Keratocyst Of Maxilla In A Nine Year Old Child - Report Of A Case Report |
Prachi Nayak 1 , Sushruth Nayak 2
1 M.D.S., Asst. Professor, Department of Oral and Maxillofacial Pathology & Microbiology - Vyas Dental College and Hospital
2 M.D.S., Asst. Professor, Department of Oral and Maxillofacial Pathology & Microbiology - Vyas Dental College and Hospital.
|
| Address For Correspondence |
Dr. Prachi Nayak, M.D.S, Assistant professor
Department of Oral and Maxillofacial
Pathology & Microbiology,
Vyas Dental College and Hospital,
Jodhpur, Rajasthan,
Phone: 09166623014
E-mail: prachi258@yahoo.co.in |
| Abstract |
| Odontogenic keratocyst (OKC) as defined by WHO are known for their peculiar behavior, varied origin, debated development, unique tendency to recur, and disputed treatment modalities. Thus, it has been the subject of much research over the last 40 years. Odontogenic keratocyst (OKC) is a cyst of tooth origin with an aggressive clinical behavior including a high recurrence rate. We report a case of nine year old female who was otherwise an healthy individual showing a recurrent odontogenic keratocyst. |
|
| Keywords |
| Odontogenic keratocyst, Recurrence. |
|
| Full Text |
Introduction:
The odontogenic keratocyst (OKC) was first described in 1876 [1]. It is one of the most aggressive odontogenic cysts of the oral cavity. OKC is known for its rapid growth [2] and its tendency to invade the adjacent tissues including bone [1, 3]. It has a high recurrence rate [3] and is associated with the Nevoid basal cell carcinoma syndrome [4]. Harring et al. best characterized this cyst by stating that "After thirty years of study, questions related to the histogenesis, pathogenesis, histology, high recurrence rate, and neoplastic potential of the OKC are still being debated" [5]. Odontogenic keratocysts are generally thought to be derived from either the epithelial remnants of the tooth germ, or the basal cell layer of the surface epithelium [6]. The majority of patients are in the age ranges of 20 to 29 and 40to 59 [7] but cases ranging from 5 to 80 years have been reported [5, 8]. In one study the average age of males was 9.7 years older than that of females [5]. The distribution between sexes varies from equality to a male to female ratio of 1.6:1, except in children [5,9]. Odontogenic keratocysts may occur in any part of the upper and lower jaw with the majority occurring in the mandible, most commonly in the angle of the mandible and ramus [5]. Odontogenic keratocysts of the maxilla are smaller in size compared to the mandible. When they are large, they tend to expand bone. No difference in site distribution was seen between unilocular and multilocular cysts [5].
Case Report:
A nine year old female patient reported with a complaint of swelling in upper left Cheek region since one week [Fig-1].
 | Fig-1: Frontal view of the patient
 |
Swelling was not associated with pain and there was no change in size since it was noted. Patient had the history of similar swelling around ten months back in the same region for which she had undergone a surgery in a government hospital. The diagnosis given was odontogenic keratocyst. The patient was otherwise healthy with an unremarkable medical history. Extra oral examination revealed a diffuse extraoral swelling located over left cheek with obliteration of nasolabial fold. The swelling was bony hard in consistency. Intra oral examination revealed a round to oval swelling located over left maxillary vestibular region covered with normal mucosa measuring 3 x 4 cm [Fig-2].
 | Fig-2: Intraoral view of the swelling
 |
On palpation the swelling was bony hard in consistency and non tender.
Intra Oral Periapical Radiograph [IOPA] revealed a well defined, unilocular radiolucency with respect to unerupted 24 [Fig-3].
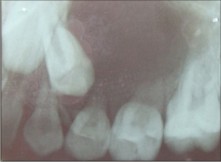 | Fig-3: Intraoral periapical radiograph showing the radiolucency in relation to unerupted 24
 |
Orthopantomogram [OPG] revealed a well defined, unilocular radiolucency with respect to unerupted 24 with distal displacement of unerupted 25 [Fig-4].
 | Fig-4: OPG of Patient
 |
Para Nasal Sinus [PNS] revealed radio opacity in left maxillary sinus [FIG-5].
 | Fig-5: PNS view of the patient
 |
The radiographic diagnosis of Dentigerous cyst was made. Complete enucleation of the cyst was done with the extraction of the associated teeth. The wound healed uneventfully. No recurrence was reported since 8 months.
The specimen was subjected to histopathological examination. Hematoxylin and eosin stained section showed the presence of cystic lining and connective tissue wall. The cystic lining showed the presence of parakeratinised stratified squamous epithelium with corrugated surface lining [Fig-6].
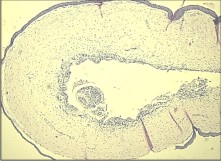 | Fig-6: Photomicrograph showing Cystic lining and connective tissue wall under 5x
 |
Basal cells were columnar with the palisading arrangement of the nuclei [Fig-7].
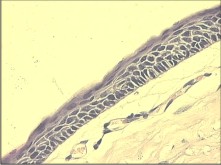 | Fig-7: Photomicrograph showing palisading pattern in basal cell layer
 |
Connective tissue showed the presence of loosely arranged collagen fibers, mild chronic inflammatory cell infiltrate with few blood vessels. The features were suggestive of Odontogenic keratocyst.
Discussion:
Though OKC is a well recognized entity, the current views on its origin vary. Some regard it as a developmental abnormality. Others consider it as a primordial cyst of a normal or supernumerary tooth before hard tissue formation. Another theory advocates the extension of basal cells from the overlying oral epithelium. Etiopathogenesis is attributed to increased mitotic activity, hydrostatic pressure, raised osmolalities, mural growth, enzymatic mechanism, bone resorbing factors, and dental lamina/proliferating basal cells.
The histological features of OKCs are characteristic. The most intriguing and renowned features is its high tendency to recur. It is said that they tend to grow more in antero-posterior direction along the cancellous component without producing much expansion of the cortical plates especially the lingual plate, for a long period of time [10]. The treatment of OKC is controversial: some authors reported low recurrence rate after enucleation, excision of overlying mucosa, curettage, and use of Carnoy's solution [11]. Most researches have advocated a strict follow-up protocol, which allows early surgical intervention in case of recurrence, limits the extent of second surgery, and thus giving rise to less morbidity [12].
In our study, the site of the swelling was maxillary upper posterior region. In the literature, there is disagreement about the most common location for maxillary OKCs. Payne [13] reported that maxillary OKCs were divided equally between the anterior maxilla and the third molar tuberosity area. Panders and Hadders [14], Pindborg and Hansen [15], Hodgkinson and colleagues [16] and Chow [17] found that there were more anterior OKCs than posterior maxillary lesions. Brannon [18], reported that the posterior region of the maxilla is the predominant site. The number of reported cases in these studies ranged from 28 to 312.
The difficulty in diagnosing OKCs based on radiographs alone has been recognized in other studies and was confirmed in our study [18]. OKCs can be mistaken easily for a dentigerous cyst radiographically like in our case. OKCs may appear as small unilocular radiolucencies [19] and may occur adjacent to a nonvital or endodontically treated tooth [20].
The main difference between OKCs and other jaw cysts are their potentially aggressive behavior. OKCs recur more often than any other type of jaw cyst [21]. The recurrence rate is almost comparable to that of the ameloblastoma [22]. The average recurrence rate is 30 percent, and a recurrence rate as high as 62 percent has been reported [15].One of the suspected contributing factors for the high recurrence rate is the presence of residual epithelium or an epithelial remnant after enucleation of the cyst [23]. Another factor is the presence of satellite cysts in the cyst's wall [24]. OKCs do not develop through an increase in osmotic pressure in the lumen, like other cysts [22]. They have an active epithelial lining with a more rapid rate of proliferation than that of radicular cysts [4]. The increased cell activity is evident by the presence of elevated level of oxidative enzymes and acid phosphatase, which indicate high metabolic and lysosomal activities [22]. In addition, OKCs' connective tissue walls have an increased level of the collagenase enzyme leucine aminopeptidase [21].
Ahlfors and colleagues [21] have proposed that OKCs should be regarded as a benign cystic neoplasm rather than a developmental cyst, and Bataineh and al Qudah [25] advocate jaw resection as the favorable treatment for an OKC. A spectrum of treatments has been recommended, ranging from enucleation to resection without a continuity defect [25]. The recurrence rate reported for resection is 0 percent; however, resection can have high morbidity [26]. The recurrence rate associated with enucleation with adjunctive therapy such as cryosurgery and decompression (1-8%) is lower than that associated with enucleation alone (17-56 percent) [26]. OKCs usually recur within five years after surgery [20], but they can recur more than 15 years later [25].
Conclusion:
Postoperative follow-up with regular radiographic examination is important with OKCs because of the high potential for recurrence.
Reference:
1. Voorsmit RACA. The incredible keratocyst. M.D. Dissertation, The Catholic University of Nijmegen, the Netherlands, 1984.
2. Broume RM. The odontogenic keratocyst - histological features and their correlation with clinical behavior. Br Dent J 1971;131:249-59
3. Stoelinga PJW, Bronkhorst FB. The incidence, multiple presentation and recurrence of aggressive cysts of the jaws. J Cranio Max Fac Surg 1988;16:184-95
4. Brannon RB. The odontogenic keratocyst. A clinicopathologic study of 312 cases. Part II. Histologic features. Oral Surgery 1977;43:233-55
5. Haring JI, Van Dis ML. Odontogenic keratocysts; a clinical, radiographic and histopathologic study. Oral Surg Oral Med Oral Pathol 1988;66:145-53
6. Hjorting-Hansen E, Andreasen JO, Robinson LH. A study of odontogenic cysts with special reference to location of keratocysts. Br J Oral Surg 1969;7:15-23
7. Brondum N, Jensen VJ. Recurrence of keratocysts and decompression treatment. A long-term follow- up of forty-four cases. Oral Surg Oral Med Oral Pathol 1991;72: 265-69
8. Anand VK, Arrowood JP Jr and Krolls. Odontogenic keratocyst: a study of 50 patients. Laryngoscope 1995;105:14-6
9. Chen CH, Lin CC. Clinical and histopathological study of the odontogenic keratocyst - a follow-up study of 16 cases. Kaohsiung J Med Sci 1986;2:601-07
10. Andras E. Longitudinal in vivo observations on odontogenic keratocyst over a period of 4 years. Int J Oral Maxillofac Surg 2001;30:80-82
11. Voorsmith RACA, Stoelinga PJW, van Haelst UJGM. The Management of Keratocysts. J Max Fac Surg 1981;9:228-236
12. Paul JW, Stoelings. Long term follow up on keratocysts treated according to defined protocol. Int J Oral Maxillofac Surg 2001;30:14- 25
13. Payne TF. An analysis of the clinical and histopathologic parameters of the odontogenic keratocyst. Oral Surg Oral Med Oral Pathol 1972;33:538-46
14. Panders AK, Hadders HN. Solitary keratocysts of the jaws. J Oral Surg 1969;27:931-8
15. Pindborg JJ, Hansen J. Studies on odontogenic cyst epithelium: clinical and roentgenologic aspects of odontogenic keratocysts. Acta Pathol Microbiol Scand 1963;58:283-94
16. Hodgkinson DJ, Woods JE, Dahlin DC, Tolman DE. Keratocysts of the jaw: clinicopathologic study of 79 patients. Cancer 1978;41:803-13
17. Chow HT. Odontogenic keratocyst: a clinical experience in Singapore. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;86:573-7
18. Brannon RB. The odontogenic keratocyst: a clinicopathologic study of 312 cases, part I-clinical features. Oral Surg Oral Med Oral Pathol 1976;42:54-72
19. Haring JI, Van Dis ML. Odontogenic keratocysts: a clinical, radiographic, and histopathologic study. Oral Surg Oral Med Oral Pathol 1988;66:145-53
20. Garlock JA, Pringle GA, Hicks ML. The odontogenic keratocyst: a potential endodontic misdiagnosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;85:452-6
21. Ahlfors E, Larsson A, Sjögren S. The odontogenic keratocyst: a benign cystic tumor? J Oral Maxillofac Surg 1984;42:10-9
22. Zachriades N, Papanicolaou S, Triantafyllou D. Odontogenic keratocysts: review of the literature and report of sixteen cases. J Oral Maxillofac Surg 1985;43:177-82
23. Rud J, Pindborg JJ. Odontogenic keratocysts: a follow-up study of 21 cases. J Oral Surg 1969;27:323-30
24. Browne RM. The odontogenic keratocyst: histologic features and their correlation with clinical behavior. Br Dent J 1971;131:249-59
25. Bataineh AB, al Qudah M. Treatment of mandibular odontogenic keratocysts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;86:42-7
26. Blanas N, Freund B, Schwartz M, Furst IM. Systematic review of the treatment and prognosis of the odontogenic keratocyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:553-8
|
|
|
|
|
|
|