Introduction:
'CARIES' has been defined as a process of enamel or dentin dissolution that is caused by microbial action at the tooth surface and is mediated by physiochemical flow of water dissolved ions. Though the disease is not life threatening, the sequels associated with it are far reaching sometimes involving systemic complications. The cost involved in treating the disease in terms of manpower and the hours spent is enormous. Therefore it is mandatory for the clinician to understand the magnitude of this problem and the risk factor in the community to plan suitable preventive measures [1].
It is surprising that in spite of enormous efforts in regard to the caries prevention there has not been a great achievement in this regard. Motivation for oral hygiene maintenance, topical fluorides diet counseling and easy access to dental facilities have helped us in controlling smooth surface caries but pit and fissure caries prevalence have more or less not changed hence the observation indicates that some of the factors are either missed, concealed or obscured in caries prevention.
Pits & Fissures, naturally occurring heaven for carious bacteria and substrates, by virtue of their anatomic shape, are extremely susceptible to caries. These deep recesses not only encourage the lesion but also limit access to salivary factors that attenuate and repair demineralization.
'PIT' is a small pinpoint depression located at the junction of developmental grooves or at the terminals of those grooves while ‘FISSURE’ is defined as deep clefts between adjoining cusps. While occlusal surfaces represent approximately 10% of the enamel surface at risk, they account for almost 50% of the caries in human dentition [1]. It has been shown that in fluoridated communities over 90% of dental caries is exclusively pit and fissure caries [2,3].
The 20th century has been witness to great strides in dentistry. The dental profession has grown and matured from an extraction oriented beginning to a sophisticated preventive philosophy. “PREVENTION IS BETTER THAN CURE”, an age old maxim which never seems to lose its relevance comes to mind. Nowhere does prevention make better sense than in the case of Dental Caries, because of its sequel involved and its widespread involvement.
Although the morphology of occlusal surfaces varies from tooth to tooth and individual to invididual, a typical premolar has a prominent primary fissure with three or four pits where as a typical molar has primary, secondary and supplementary fissures with as many as 10 pits, this accounts for the higher prevelence of pit and fissure caries in molars when compared to premolars.
A giant step towards this goal has been the use of fluorides. But fluorides essentially take care of only the tip of the iceberg, smooth surface caries, leaving Pit & Fissure Caries, which accounts for nearly 2/3 of the carious experience with little prevention. A Pediatric dentists primary goal, amongst many, is Prevention, before insidious onset of diseases and fostering of lifelong positive health habits so that dental and oral structures will be maintained in optimal condition as long as possible.
The aim of this paper was to review the literature for the different aspects of pit and fissure caries and its prevention.
Methodology
The review has drawn on the search strategy from various electronic databases, like Medline (pubmed), Science direct, Wiley interscience and Ebscohost. These databases represent the most often searched databases for carrying out medical systematic reviews. 63 articles were selected based on critical evaluation criteria and were reviewed.
EPIDEMIOLOGY OF PIT & FISSURE CARIES
During 1970’s observation revealed that 70% of all molar occlusal surfaces became carious within 10 years of emergence into oral cavity while a high percentage of these occlusal lesions occurred in the first 3 years after eruption [4]. There has been a predominant reduction in number, intensity, speed of caries attack on smooth surface as compared to that of occlusal surface. Tooth surfaces with pits & fissures are particularly vulnerable to caries
development[5] as observed that although occlusal surfaces represented only 13% of total surfaces of the permanent dentition, they accounted for almost 88% of caries in children [6]. The drastic reduction in dental caries seen over the past few decades as a result of fluoridation has had little effect on pit & fissure caries as it had been reported that in fluoridated communities over 90% of dental caries is exclusively pit and fissure caries [7,8] Approximal smooth surface caries reduction was attributable to 50 percent post-eruptive fluoride exposure, whereas pit and fissure caries reduction was attributable to 33 percent post-eruptive fluoride exposure [9]. The increased proportion of caries experience attributed to pit & fissure caries is due to the decreasing prevalence of inter proximal caries.
Prevalence
Dental caries is a rapidly emerging oral health problem amongst the children of India, its incidence in different states varies between 31% and 89% . An overall caries prevelence of 77.7% was recorded which is 67.26% in the age group of 7-9 years and 80.86% in 10-12 years with DMFT+deft of 1.97 band 2.61 respectively and also observed that greater treatment needs in older age groups. Significant finding revealed that 59.96% required restorative treatment out of the various dental treatment needs [10].
Other studies showed the prevelence data for dental caries was 85.5%, 88.9%, 70.6% in 7-8, 9-10, 12 years old respectively with prevelence of dental caries in permanent molar increased with age and became as high as 57.7% in 12 years old children [11]. An analysis of Irish data collected in 1997 shows that, for 15-year-olds in non-fluoridated areas, 72% of the DMFS of 6.1 occur on occlusal surfaces.
Nagano [12] classified occlusal fissures into five types (figure 1) on the basis of fissure morphology: With V-type (34%), U-type (14%), I-type (19%), IK-type (26%), Inverted Y-type (7%).
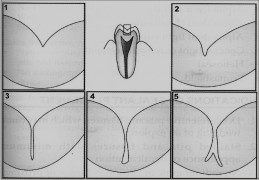 | Figure 1- Type of fissures
 |
Current trends in untreated caries: This decline in the untreated caries may reinforce the already apparent shift from restorative to preventive dental services.
In Primary Dentition the overall decline for the age 2-10 years has been documented to be 55.6% in untreated carious teeth and 58% in the carious surface. In which 2-5 years have shown 30.2% and 6-10years old have shown 63.7% decline in untreated carious teeth. The decline was seen more among boys (60.0%) compared to girls (50.0%) [13]. Approximately 1/3 of children between ages 1 and 3 years have experienced caries in the primary dentition and caries in occlusal surface may account for upto 67% of lesions.
In Permanent Dentition the prevalence of decayed or filled occlusal surfaces on permanent first molars in 10-year-old children dropped from about 55% to about 15% between national surveys in 1971-1974 and 1988-1994 [14]. A 40 month study by Stall & Katz (1992) among 16-22 years showed that 32.9% developed occlusal caries without radiographic interproximal lesions in permanent molar and premolars and 9.8% developed occlusal caries with radiographic interproximal lesions in permanent molar and premolars. He concluded that sealant placement could have prevented 75% of the lesions.
In another survey prevalence of decayed or filled occlusal surfaces on permanent second molars in 16-year-old children dropped from about 68% to about 25% between 1971-1974 and 1988-1994 [14]
DIAGNOSIS OF PIT & FISSURE CARIES
In 1968, at an ADA sponsored conference on clinical testing of cariostatic agents the criteria for detection and diagnosis of pit & fissure lesions were defined as follows [15]:
Caries is present when the explorer catches or resists removal after insertion into a pit or fissure with moderate to firm pressure and when this is accompanied by one or more of the following signs of caries.
a) Softness at base of the area.
b) Opacity or loss of normal translucency adjacent to a pit or fissure as evidence of undermining or remineralization.
c) Softened enamel adjacent to the pit or fissure that can be scraped away with the explorer.
But the diagnosis of pit & fissure caries consistently presents with the following problems.
1) Clinical examination is quite variable from one practitioner to another owing to size and shape of explorer tip, the force applied and the judgment of the examiner [16].
2) Radiographic evaluation of occlusal surfaces has been found to be of minimal diagnostic value in detecting enamel caries and superficial dentinal caries [17].
3) Transillumination has been of value of interproximal surfaces but has failed to provide additional information about the caries status of occlusal surfaces [18]
4) As a possible answer to all these problems, during the 1980’s, and ancillary diagnostic device, “Electronic Caries Detector” was introduced. It was touted to be superior to the explorer because of its increased sensitivity, specificity and consistency [19]. In laboratory studies comparing the clinical, radiographic and histologic appearances of occlusal caries, the electronic caries detector was found to correlate well with the extent of histologic involvement [20]. However, because of the expense of the instrument and the paucity of clinical studies, the electronic caries detector has not been widely accepted.
At this time, diagnosis of pit & fissure caries is based on visual assessment using a mouth mirror and adequate lighting and tactile examination with a sharp explorer. The most important elements in diagnosis of and treatment planning for pit & fissure caries are CLINICAL JUDGEMENT AND EXPERIENCE.
PREVENTION OF PIT & FISSURE CARIES
Historical Perspective And Sealant Materials
Prophylactic Restoration
In 1924, Thaddeus Hyatt advocated prophylactic restoration. This procedure consisted of preparing a conservative class I cavity that included all pits & fissures at risk for caries development and then placing an amalgam restoration. The rationale for prophylactic restoration of an otherwise caries free surface was that it prevented further insult to the pulp, decreased loss of tooth structure and less time for restoration when tooth eventually succumbed to caries.
Prophylactic Odontotomy and Fissure eradication
This conservative approach was advocated by Bodecker in 1929. Initially he advocated cleansing the fissure with an explorer and flowing a thin mix of oxyphosphate cement in to the fissure in order to seal it. Later he advocated prophylactic odontotomy, which involved mechanical eradication of fissures into cleansable ones.
Pit & Fissures Sealants:
Different type of sealant materials in the current context:-
a) Resin based sealants
b) Glass ionomer sealants
Bunocore (1955) advocated the filling of pit and fissures with bonded resin based sealants. The development of pit & fissure sealants was based on the discovery that etching enamel with phosphoric acid increased the retention of resin restorative materials and improved marginal integrity considerably.
First Sealant:
The first sealant material that utilized the acid etch technique was the cyanoacrylate substance (mid 1960’s). But this was not suitable as a sealant owing to bacterial degradation of the material in the oral cavity over time.
ADVANCEMENTS
Bowen (1965) reported BIS-GMA a viscous resin was found to be resistant to degradation and produced a tenacious bond with etched enamel, a resin formed by reacting bisphenol A with glycidyl methacrylate. Various types of pit and fissures are available in the market, depending upon the type of polymerization, type of light care used, color, filler particles etc.
Even Glass Ionomer Cement has been advocated for the use of pit and fissure sealants (self cure type). However, it is advisable to select a ionomer based sealants if moisture free area cannot be achieved [21,22], but, this is considered a temporary measure only [22,23]. Some of the studies concluded that retention for resin bases sealants is better than for the Glass Ionomer sealant but difference in caries prevention remain equivocal [24], while some of the studies contradicted with resin based composites performing better in preventing dentin lesions [25,26]. But if length of retention of sealant was considered a proxy to increased caries prevention in pit and fissure, resin based sealants scores better.
Other methods for the prevention of pit and fissure caries which have been investigated are
Lasers It was hypothesized that thermal treatment with lasers converts the carbonated hydroxyapatite of tooth enamel to a less soluble mineral, and chemical inhibitors work by a common ion effect of the fluorapatitic surface, which is more effective on the less soluble laser modified enamel. Another explanation proposed is carbonate loss, which is a soluble mineral that is lost from the carbonated apatite tooth mineral during specific laser irradiation [27,28]. This reduced carbonate content could decrease demineralization of the substrate, because of a poorer fit of carbonate in the lattice, generating a less stable and more acid-soluble apatite phase. There is no consensus with regard to whether the fluoride treatment should be performed before or after laser irradiation. However, all experiments associating CO2 laser irradiation and fluoride treatment showed better results in caries prevention when compared to one single treatment. Therefore such ‘combination therapy’ may be clinically effective.
GC Mousse- Casein-phosphopeptide_stabilized amorphous calcium phosphate nanocomplexes (CPP-ACP) have anticariogenic properties and significantly increase the quantities of calcium and phosphate ions in supragingival plaque. The ability of CPP-ACP plus fluoride ions to increase the incorporation of fluoride into supragingival plaque and subsurface enamel, thereby leading to enamel remineralization with acid-resistant mineral, substantially increased the remineralization of subsurface lesions of enamel compared to the results with fluoride alone [29]. The combination of CPP-ACP and fluoride appears to be a better choice for reducing caries risk than using fluoride alone or bioactive glasses based on calcium sodium phosphosilicate compounds [30], know as Novamin (CSP). Casein phosphopeptide (CPP) stabilizes calcium phosphate by binding to amorphous calcium phosphate (ACP), thus forming CPP-ACP clusters. These clusters serve as reservoirs for calcium and phosphate and cling to dental plaque and tooth surfaces. An acidic challenge prompts the release of calcium and phosphate ions, producing a supersaturated mineral environment and enhancing remineralization while minimizing demineralization [31].
Fluoride varnish- On the other hand, fluoride varnishes are another option, although imported varnishes cost four to eight times more than national ones. However, several reports
have confirmed their effectiveness [32,33,34,35] other studies have shown reductions of 28% to 52% in the depth of lesions after the application of fluoride varnish [33,36]. Clinical evaluation of the comparison between preventive effect of fluoride varnish and gel revealed better cariostatic results with varnishes. The most recent Cochrane reviews [37] concluded that there was some evidence that pit and fissure sealants are superior to fluoride varnishes for the prevention of occlusal caries.
Preventive resin restoration – a conservative answer to ‘extension for prevention’ philosophy. It integrates the preventive approach of occlusal sealant therapy for caries susceptible pits and fissures with the therapeutic restoration of incipent caries that occur in the same occlusal surface with composite resin. Preventive resin restoration is the nomenclature that has been historically used used; however, this terminology has been replaced by “Conservative Adhesive Restoration” to reflect the fact that other adhesive material may be utilized in these restorations. This updated term was first described by Simonsen and Stallard in 1977 [38] and refined in 1985 [39].
Pit and fissure sealant with ACP – light cure material that contains ‘smart material’ Amorphous Calcium Phosphate which is more flexible, resilient, creating a stronger and long lasting sealant.
Fissurotomy – Bodecker, 1929, who suggested widening the fissures mechanically so that they would be less retentive to food particles
DISCUSSION
The high susceptibility of pit and fissure to caries presents a major dental problem and provides a rationale for caries control of these areas. In the contemporary cariology, there is a paradigm shift from the concept that carious tissue should be removed before a tooth with a carious lesion is restored, towards the view that a carious lesion can be sealed and, thus, be arrested [40]. Placement of occlusal sealants is a, “SPECIFIC PROTECTION”, procedure in “PRIMARY PREVENTION”. One of the first recorded recommendations in the use of a preventive measure for occlusal caries was by Gabell in 1941 [41]. Pit & Fissure Sealant is an example of disease prevention based on a sound ecological principle and that is what dentistry in the 21st century is all about. Also reported evidences suggested that there had been a drastic caries reduction for fissure sealant ranging from 86% at 12 months to 57% at 48-54 months 42 and depending upon the type of sealant used [43,44] and duration of retention.
A study was done to evaluate the influence of fissure morphology on the adhesion and penetration of pit and fissure sealants, shows that the depth of penetration was comparable in V-shaped and U-shaped fissures and was found to be better than in other shapes. For I and IK-shaped fissures, the level of penetration was again found to be almost similar and poorest than in the other shapes. For Y-shaped fissures, the depth of penetration was less than that for U and V-types but more than that for I and IK-types. Obturation of these anatomical faults by occlusal sealants greatly reduces number of cariogenic bacteria in the mouth, an excellent example of ecological control of undesirable plaque organisms without wholesale disruption of remainder of the oral flora and also prevents retention of cariogenic substrate [45].
Finally, SEM study (Figure 2) showed that sealants are superior as they occlude the fissures without any gap and with least probability of microleakage and hence found to be superior material in comparison to latest remineralizing agents [45].
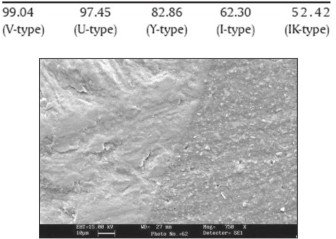 | Figure 2- SEM picture showing sealant enamel interface without any gaps
 |
It has been seen that sealant retention has been of paramount importance in the effective prevention of carious lesion. The presence of prismless layer of enamel at the fissure entrance and fissure walls [46,47], along with the presence of organic material within the fissure [48] and the air bubbles trapped inside the fissure [49] resulted in reduced etching pattern and decrease sealant penetration in many instances leading probably to early loss.
A study on the effective means of etching primary prismless enamel [50] showed that grinding of the enamel by the use of handpiece should be followed by etching of the enamel.
Considering the material factor, resin bonded sealants proved to be more efficient due to their higher retention rate as their counterpart Ionomer sealants [51,52,53]. Study comparing the acid etching with bur showed a higher retention rate with acid etching [54] Retention also proved to be improved by the use of hydrophilic single primer prior to light cured resin bonded sealant [55]. In a split mouth design study unfilled light cured resin bonded sealant was significantly better retained than filled one [56].
Considering all the factors pit and fissure sealants have shown far promising results than rest of the caries preventive techniques. A study in a fluoridated community, molars scored initially as sound became carious at the rate of 13% if not sealed and at a rate of 8% if sealed. Molars scored initially as incipient or questionable became carious at a rate of 52% if not sealed and a rate of 11% if sealed, there by representing striking protective effect. Delta dental data analysis center revealed 85% fewer carious lesions on all tooth surfaces when molar surfaces were sealed in a 4 years study [57].
One the major barrier to providing sealants is the concern about inadvertently sealing over caries [58,59]. Another report found that dental sealants reduced the probability of caries progression by more than 70% compared to untreated control teeth [60]. But still the findings indicated that cavitated caries fissures cannot be sealed as adequately as sound fissures due to presence of biofilms left in the deeper parts, which are difficult to assess [40].
All the guidelines agree that to achieve the greatest possible caries reduction; a comprehensive caries preventive program must use sealants in conjunction with other caries preventive methods, such as systemic and topical fluorides, sound dietary habits and proper oral hygiene (ADA, 1987). Sealants were shown to be more effective and providing cost saving if placed in patients with a high rather than low caries risk [61,62,63].
Conclusion
Sealants are an important dental caries prevention technology, ideally used in combination with patient education, effective personal oral hygiene, fluorides and regular dental visits.
Recommendations
The following recommendations are based on the evidence gathered in this review:
1. Sealants should be placed on all permanent molar teeth without cavitation as soon after eruption as isolation can be achieved.
2. Sealants should be placed on the primary molars of children who are susceptible to caries (i.e., those with a history of caries).
3. Resin bonded sealants should be preferred, until such time as GIC sealants with better retention capacity are developed.
4. Sealants should be placed as part of an overall prevention strategy based on assessment of caries risk. Other preventive measures include application of fluoride varnish, education, nutritional counselling and regular clinical review (at least annually, but semiannually wherever possible).
References
1. Tandon S, Bhalla S. Introduction – Dental caries in early childhood. In: Tandon S, editors. Textbook of pedodontics. IInd ed. Paras medical publisher, 2009: 183-191.
2. Brown LJ, Kaste LM, Selwitz RH, Furman LJ. Dental caries and sealant usage in U.S. children, 1988-1991: selected findings from the Third National Health and Nutrition Examination Survey. J Am Dent Assoc 1996;127(3):335-43.
3. Kaste LM, Selwitz RH, Oldakowski RJ, Brunelle JA, Winn DM, Brown LJ. Coronal caries in the primary and permanent dentition of children and adolescents 1-17 years of age: United States, 1988-1991. J Dent Res 1996;75(special issue):631-41.
4. Carlos JP, Gittelsohn AM. Longitudinal studies of the natural history of caries—II: A life-table study of car¬ies incidence in the permanent teeth. Arch Oral Biol 1965;10:739-751.
5. Manton DJ, Messer LB. Pit and fissure sealants: another major cornerstone in preventive dentistry. Aust Dent J 1995;40(1):22-9.
6. Brown LJ, Selwitz RH. The impact of recent changes in the epidemiology of dental caries on guidelines for the use of dental sealants. J Publ Health Dent 1995;55(special issue):274-291.
7. Brown LJ, Kaste LM, Selwitz RH, Furman LJ. Dental caries and sealant usage in U.S. children, 1988-1991: selected findings from the Third National Health and Nutrition Examination Survey. J Am Dent Assoc 1996;127(3):335-43.
8. Kaste LM, Selwitz RH, Oldakowski RJ, Brunelle JA, Winn DM, Brown LJ. Coronal caries in the primary and permanent dentition of children and adolescents 1-17 years of age: United States, 1988-1991. J Dent Res 1996;75(special issue):631-41.
9. Newbrun E. Topical Fluorides in Caries Prevention and Management: A North American Perspective. J Dent Educ. 2001;65(10):1063-72.
10. Grewal H, Verma M, Kumar A. Prevalence of dental caries and treatment needs in the rural child population of Nainital District, Uttaranchal. J Indian Soc Pedod Prev Dent. 2009;27(4):224-6.
11. Saldunaite K, Puriene A, Milciuviene S, Brukiene V, Kutkauskiene J. Analysis of dental caries prevention program in 7-12-year-old Lithuanian schoolchildren. Medicina (Kaunas). 2009;45(11):887-95.
12. Nagano T. Relation between the form of pit and fissure and the primary lesion of caries. Dent Abstr 1961;6:426.
13. Brown LJ, Wall TP, Lazar V. Trends in untreated caries in primary teeth of children 2 to 10 years old. J Am Dent Assoc 2000b;131:93-100.
14. Feigal RJ, Donly KJ. The use of pit and fissure sealants. Paediatr Dent 2006;28:143-150
15. Radike A. Criteria for diagnosis of dental caries; Proceedings of the conference on clinical testing of cariostalic agents; 1968, Chicago : American Dental Association.
16. Houpt M, Fuks AB, Eidelman E. Measuring the stickiness of pits and fissures in enamel. Clin Prev Dent. 1985;7(3):28-30.
17. Mcknight-Hanes C. Myers DR, Dushku JC. Radiographic recommendations for the primary dentition: comparison of general dentists and paediatric dentists. Pediatr Dent 1990;12(4):217-21.
18. Rock, WP J. The diagnosis of early carious lesions -- a review. Paediatr Dent 1987;3,1-6.
19. White GE, Tsamtsouris A, Williams DL. A longitudinal study of electronic detection of occlusal caries. J Pedodont 1981;5(2):91-101.
20. Flaitz CM, Hicks MJ, Siverstone LM. Radiographic, histologic, and electronic comparison of occlusal caries: an in vitro study. Pediatr Dent 1986;8:24-28.
21. Locker D, Jokovic A, Kay EJ. Prevention. Part 8: The use of pit and fissure sealants in preventing caries in the permanent dentition of children. Br Dent J 2003;195:375–8.
22. Smallridge J. UK national clinical guidelines in paediatric dentistry. Management of the stained fissure in the first permanent molar. Int J Paediatr Dent 2000;10:79–83.
23. Aranda M, Garcia-Godoy F. Clinical evaluation of the retention and wear of a light-cured pit and fissure glass ionomer sealant. J Clin Pediatr Dent 1995;19:273–7.
24. Simonsen RJ. Glass ionomer as fissure sealant – a critical review. J Public Health Dent 1996;56:146–9.
25. Raadal M, Utkilen AB, Nilsen OL. Fissure sealing with a light-cured resin-reinforced glass-ionomer cement (Vitrebond) compared with a resin sealant. Int J Paediatr Dent 1996;6:235–9.
26. Rock WP, Foulkes EE, Perry H, Smith AJ. A comparative study of fluoride-releasing composite resin and glass ionomer materials used as fissure sealants. J Dent 1996;24:275–80.
27. Featherstone JBD, Barrett-Vespone NA, Fried D, Fried D, Kantorowitz Z, Seka W. CO2 laser inhibitor of artificial caries like lesion progression in dental enamel. J Dent Res 1998;77:1397-403.
28. Featherstone JDB. Caries detection and prevention with laser energy. Dent Clin North Am. 2000 Oct;44(4):955-69
29. Reynolds EC, Cai F, Cochrane NJ, et al: Fluoride and casein phosphopeptide- amorphous calcium phosphate. J Dent Res 2008;87:344-348.
30. Featherstone JD, Rapozo-Hilo ML, Rechmann P, Rechmann B, Greenspan D. In vitro root caries inhibition by phosphosilicate and fluoride dentifrices. Abstract 0501 – IADR – 2007.
31. Yengopal V, Mickenautsch S: Caries preventive effect of casein phosphopeptide-amorphous calcium phosphate (CPP-ACP): A meta-analysis. Acta Odontol Scand 2009;67:321-332.
32. Eronat C, Eronat N, Alpoz AR. Fluoride uptake by enamel in vitro following application of various topical fluoride preparations. J Clin Pediatr Dent. 1993;17(4): 227-30.
33. Ogaard B, Duschener H, Ruben J, Arends J. Microradiography and confocal laser scanning microscopy applied to enamel lesions formed in vivo with and without fluoride varnish treatment. Eur J Oral Sci. 1996;104(4):378-83.
34. Schmidt JL, Staley RN, Wefel JS, Kanellis M, Jakobsen JR, Keenan PJ. Effect of fluoride varnish on demineralization adjacent to brackets bonded with RMGI cement. Am J Orthod Dentofacial Orthop. 2002;122(2):125-34.
35. Shobha T, Nandlal B, Prabhakar AR, Sudha P. Fluoride varnish versus acidulated phosphate fluoride for schoolchildren in Manipal. J Indian Dent Assoc. 1987;59(6-9):157-60.
36. Hicks J, Wild T, Flaitz CM, Seybold S. Fluoride and caries development in primary tooth enamel: an in vitro study. ASDC J Dent Child. 2001;68(5-6):304-10.
37. Hiiri A, Ahovuo-Saloranta A, Nordblad A, Makela M. Pit and fissure sealants versus fluoride varnishes for preventing dental decay in children and adolescents. Cochrane Database Syst Rev 2006; (4):CD003067.
38. Simonsen RJ, Stallard RE. Sealant –restoration utilizing a dilute filled resin: One year results. Quintescence Int 1977:8(6); 77-84
39. Simonsen RJ. Conservation of tooth structure in restorative dentistry. Quintescence Int 1985:16(1);15-24.
40. Amerongen JPV, Davidson CL, Opdam NJM, Roeter FJM, Kidd EAM. Restoring the tooth: ‘the seal is the deal’. In: Fejerskov O, Kidd EAM, editors. Dental caries: the disease and its clinical management. Ist ed. Oxford: Blackwell Munksgaard, 2003: 275-290.
41. Gabell AB. Operative Procedures. In: ML Ward, editors. The American Textbook of Operative Dentistry. Ist ed. London: Henry Kimpton, 1941:346-347.
42. Azarpazhooh A, Main PA. Pit and fissure sealants in the prevention of dental caries in children and adolescents: a systematic review. J Can Dent Assoc 2008;74:171–7.
43. Llodra JC, Bravo M, Delgado-Rodriquez M, Baca P, Galvez R. Factors influencing the effectiveness of sealants—a meta- analysis. Community Dent Oral Epidemiol 1993;21:261–8.
44. Beiruti N, Frencken JE, van’t Hof MA, van Palenstein Helderman WH. Caries-preventive effect of resin-based and glass ionomer sealants over time: a systematic review. Community Dent Oral Epidemiol 2006;34:403–9.
45. Grewal N, Chopra R. The effect of fissure morphology and eruption time on penetration and adaptation of pit and fissure sealants: An SEM study. J Indian Soc Pedod Prev Dent. 2008;26(2):59-63
46. Burrow MF, Burrow JF, Makinson OF. Pits and fissures: Etch resistance in prismless enamel walls. Aust Dent J 2001;46:258-262.
47. Hoh A, Ngo H, Mount GJ, Morris M, Baker C. A SEM study of tooth morphology using high KV and back scattered Electron Imaging Technique. J Dent Res 2000;80:973.
48. Burrow MF, Makinson OF. Pits and fissures: remnant organic debris after acid-etching. ASDC J Dent Child 1990;67:348-351.
49. Juhl M. Three-dimensional replicas of pit and fissure morphology in human teeth. Scand J Dent Res 1983;91:90-95.
50. Hosoya Y, Johnston JW. Evaluation of various cleaning and polishing methods on primary enamel. J Pedod 1989;13:253-269.
51. Arrow P, Riordan PJ. Retention and caries preventive effects of a GIC and a resin-based fissure sealant. Community Dent Oral Epidemiol 1995;23: 282–5.
52. Forss H, Saarni UM, Seppa L. Comparison of glass– ionomer and resin-based fissure sealants: a 2-year clinical trial. Community Dent Oral Epidemiol 1994;22:21–4.
53. Poulsen S, Beiruti N, Sadat N. A comparison of retention and the effect on caries of fissure sealing with a glass–ionomer and a resin-based sealant. Community Dent Oral Epidemiol 2001;29:298–301.
54. Lygidakis NA, Oulis KI, Christodoulidis A. Evaluation of fissure sealant retention following four different isolation and surface preparation techniques: four-year clinical trial. J Clin Pediatr Dent 1994;19:23–5.
55. Soh JM, Punwani IC, Soh N, Ha CY, Koerber A. Efficacy of dual-cure sealant with bonding primer. J Dent Res 2002;81:A71 (Abstract).
56. Rock WP, Weatherill S, Anderson RJ. Retention of three fissure sealant resins. The effects of etching agent and curing method. Results over 3 years. Br Dent J 1990;168:323–5.
57. Heller KE, Reed SG, Bruner FW, Eklund SA, Burt BA. Longitudinal evaluation of sealing molars with and without incipient dental caries in a public health program. J Publ Health Dent 1995;55:148-153.
58. Chapko MK. A study of the intentional use of pit and fissure sealants over carious lesions. J Publ Health Dent 1987;47(3):139-142.
59. Primosch RE, Barr ES. Sealant use and placement techniques among pediatric dentists. J Am Dent Assoc 2001;132(10): 1442-1451.
60. Griffin SO, Oong E, Kohn W, et al. The effectiveness of sealants in managing carious lesions. J Dent Res 2008;87(2):169-174.
61. Ahuovuo-Saloranta A, Hiiri A, Nordblad A, Mäkelä M, Worthington HV. Pit and fissure sealants for preventing dental decay in the permanent teeth of children and adolescents. Cochrane Database Systematic Review 2008;4:CD001830.
62. Weintraub JA. Pit and fissure sealants in high-caries-risk individuals. J Dent Edu 2001;65:1084–90.
63. Simecek JW, Diefenderfer KE, Ahlf RL, Ragain JC. Dental sealant longevity in a cohort of young U.S. naval personnel. J Am Dent Assoc 2005;136:171–8 |