INRODUCTION:
There is one place where children dread to go, it is the dentist's chair. The sight of a large syringe being injected into tender gums can bring tears to the eyes of most of the children.. An ideal extraction is the painless removal of the entire tooth with minimal trauma to the investing tissues, so that the wound heals uneventfully. The extraction of tooth is an emotionally upsetting to the child and parents, thus it need to be rectified by use of certain modifications. Thus, effective pain control in children during dental treatment is important to achieve comfort, cooperation, and compliance with dental care during adulthood. For invasive procedures such as teeth extraction, local anaesthesia is administered.1 This involves the injection of an anesthetic to block sensation to the nerve that sends pain signals to the brain. By blocking the nerve with an anesthetic, the dentist numb the area requiring treatment for a specific period of time. But the thought of having a needle inserted into your cheek bring tears to the eyes of children. may be a source of pain, discomfort, and distress for children, parents, Dentistry has come a long way over the last few years to eliminate the discomfort associated with injections. Different methods have been proposed to alleviate this pain.2
Topical Anesthesia (or "numbing gel") is commonly used to numb tissues before an injection, so that one can't feel the needle glide in. But topical application of local anesthetic agents may not have adequate clinical effect for certain procedures in pediatric dentistry3
One of the most critical factors in topical anesthetic is maintaining prolonged intraoral mucosal contact. Most topical anesthetic agents used in dentistry come in gel form, which can be difficult to localize to a particular site and are easily diluted by saliva.
Therefore newer techniques are introduced The purpose of this article is to review the niche applications of these techniques and to summarize the scientific literature appraising their use. Some of latest techniques are discussed below.
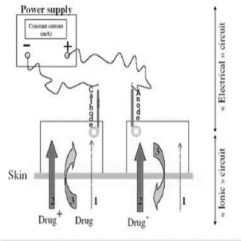
Iontophoresis
Recently there has been an increased interest in using iontophoretic technique for the transdermal delivery of medications, both ionic and nonionic.
The method of iontophoresis was described by Pivati in 1747. Galvani and Vota two well known scientists working in the 18 th century combined the knowledge that the electricity can move different metal ions and the movement of the ions produce electricity Iontophoresis is defined as the introduction, by means of a direct electrical current of ions of soluble salts into the tissue of the body for therapeutic purposes. It is a technique used to enhance the absorption of drugs across biological tissues such as the skin4.
Iontophoresis is the method where the movements of ions across a membrane enhanced using an externally applied potential difference. When the membrane under consideration is skin, the method is called transdermal iontophoresis5. The principle barrier to the transport of the molecules into an across the skin is stratum corneum (SC), this is the uppermost layer of the epidermis with a thickness of between 10-100 µm. The SC consists of several layers of corneocytes (a nucleate keratin filled cells) inlaid in a lipid matrix, a continuous medium through the SC, arranged mainly in bilayers5,6. The intercellular lipids consist of approximately equal quantities of ceramides, cholesterols and free fatty acids. Percutaneous absorption may take place simultaneously by any combination of the three main pathways that include; the intercellular (paracellular) pathway between the corneocytes along the lamellar lipids, the intracellular (transcellular)
pathway through the cells or the appendageal (shunt) pathway via hair follicles, sweat ducts and secretary glands.Ions prefer the routes of the least electrical resistance; in the SC this is believed to be via the pores. Some investigations indicate that these pores are sweat glands , others that transport occurs through both hair follicle and sweat glands. Iontophoretic delivery of lignocaine 2% was effective in reducing the pain of venipuncture and venous cannulation within 10 minutes. Tharian ad Tandon 1993 found iontophoresis a suitable alternative of the drug for achieving surface anaesthesia . It presents a painless modality for administration of anaesthesia. (Fig 1)
 |
 |
FIG 1: IONTOPHORESIS
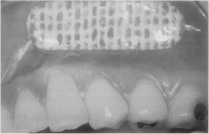
Intraoral patch.
To reduce the perception of pain associated with needle penetration, dentists often apply topical anesthetics to the oral mucosa before injecting local anesthetic solutions.7 While a number of placebo- controlled clinical trials have studied the effectiveness of such topical agents, and found that one of the most critical factors in topical anesthetic is maintaining prolonged intraoral mucosal contact
Thus, dentistry would benefit from the development of a topical anesthetic system that could adhere to the oral mucosa, maintain effective local anesthetic concentrations and demonstrate efficacy even when the local anesthetic was administered with 25-gauge needles and the periosteum was contacted Anesthetic patches containing lidocaine base that is dispensed through a bioadhesive matrix and applied directly to the oral mucosa recently have been approved by the Food and Drug Administration and are commercially available (DentiPatch lidocaine transoral delivery system, Noven Pharmaceuticals Inc.)8,9. These patches are available in 10 and 20 percent concentrations, each containing approximately 23 and 46 milligrams of lidocaine base per 2 square centimeters of patch, respectively. The lidocaine contained in the matrix diffuses directly through the mucosa while the patch is affixed. ( Fig 2)
 |
 |
FIG 2: INTRAORAL PATCH
Jet injection
Many devices have been developed that would eliminate the need to inject material by needle and syringe. The development of jet injectors was one of the first fundamental improvements. First described in 1866, jet-injection devices were originally developed for mass immunization10. Modern designs have been approved for intramuscular and subcutaneous delivery of medications such as hepatitis B vaccine and insulin. Needleless jet injectors such as the Syrijet Mark II system (Mizzy Inc., Cherry Hill, NJ) are marketed for use in the dental setting.11 A jet injector is a type of medical injecting syringe that uses a high-pressure narrow jet of the injection liquid
instead of a hypodermic needle to penetrate the epidermis, the purpose being to reduce the pain associated with needle injection12. The advantages of needleless systems for delivery of local anesthetic include rapid onset of anesthesia, predictable topical anesthesia of soft tissues, controlled delivery of anesthetic dose, obviation of needle-stick injury, obviation of intravascular injection and high patient acceptance, especially in instances of needle-phobia. (Fig 3)
FIG 3: JET INJECTION
Computer controlled injections
There are currently a number of computer-controlled injection devices available. Compared to a standard syringe, computer-controlled injection devices are larger, require more operatory space. Because the needle and handle generally appear less threatening and are more aesthetic, patient acceptance is generally high. The ability of the computer to control and limit the rate of the injection and subsequently limit patient discomfort has created considerable popularity for these devices13. Wand was the first computer-controlled dental anesthetic delivery system.The Wand Local Anesthesia System is a computer controlled injection device, the size of a paperback book. It accommodates a conventional local anesthetic cartridge that is linked by microtubing to a disposable, lightweight, pen like handle with a Luer lock needle attached. The computer-controlled system is activated by a foot control that automates the delivery of local anesthetic at a precise pressure and volume ratios, resulting in an effective and comfortable injection. Patients who have experienced an injection with this system report a virtually imperceptible needle penetration followed by a sensation of mild pressure. It has been reported that the physical appearance of dental injectors is important to children and even more important for children who are anxious.14.The manufacturer suggests that needle penetration and advancement be done very slowly to allow for anesthetic to proceed along the path of the needle. The Wand/CompuDent system administers local anesthetic at two specific rates of delivery. The slow rate is 0.5 mllmin and the fast rate is 1.8 mb’min. An aspiration test can be activated at anytime by simply releasing the pressure on the foot-rheostat starting a 4.5-second aspiration cycle. The Wand/CompuDent system permits both a precise rate of flow and a controlled pressure to be maintained irrespective of the type of tissue into which the local inesthetic is being deposited. Therefore even tissues with low elasticity receive a constant pressure and rate of flow, resulting in a more favorable (e.g., comfortable, less tissue damage) outcome. The controlled rate of fluid administration also explains e reduced pain perception noted by most patients during dental injections into tissues that typically elicit a high pain response (e.g., the hard palate, attached gingiva, and periodontal ligament). (Fig 4)
FIG 4: WAND
Comfort Control Syringe
Introduced several years after the Wand, the Comfort Control Syringe (CCS) system attempts to improve on the CCLAD concept. The CCS system is an electronic, preprogrammed delivery device that provides the operator with the control needed to make the patient’s local anesthetic injection experience as pleasant as possible. CCLADs, this is achieved by depositing the local anesthetic more slowly and consistently than is possible manually. The CCS has a two- stage delivery system; the injection begins at an extremely slow
rate to prevent the pain associated with quick delivery. After 10 seconds. the CCS automatically increases speed to the preprogrammed injection rate for the technique selected. There are five :preprogrammed injection rates for specific injections. The front button with the arrow and square controls the “Start/Stop” functions by initiating or terminating the selected program. The middle button activates the “Aspiration” function by slightly retracting the plunger15. The rear button initiates “Double Rate” and operates in the same manner as the Double Rate button on the unit. It doubles the preprogrammed injection rate. Selecting it again resumes the preprogrammed speed.
Electronic Dental Anesthesia
This method of achieving local anesthesia involves the use of the principle of Transcutaneous Electrical Nerve Stimulation (TENS) which causes the relief of pain. It can be used as a supplement to conventional local anesthesia and has been found to be well accepted by the parents. Electronic dental anesthesia requires a considerable degree of patient cooperation and participation to be successful. With this in mind, the use of EDA in younger populations, although not contraindicated, requires a more intensive evaluation of patients’ abilities to both understand the concept of EDA and to perform their tasks properly. The physiological basis of pain relief due to TENS has been attributed to the activation of large-diameter primary
afferent beta fibers (sense of touch) that segmentally inhibit central pathways through a gating mechanism. The release of opioid peptides (endorphins and enkephalins) and other neurochemicals, such as 5-hydroxytryptamine, has also been implicated The electronic dental anesthesia apparatus (Electro-Med Dental Anaesthesia 14S, Electro-Med Box Hill, Victoria, Australia) was used.16 This device produces a postsynaptic, exponentially decaying wave with a maximum frequencyof 500 Hz, a maximum amplitude of 23 V and a pulse width of 130 us. It also generates a bipolar square wave with a maximum frequency of 500 Hz, a maximum amplitude of 25 V and a pulse width of 100 us.
EMLA
In recent years, a new topical anesthetic agent has been developed, EMLA cream 5% (eutectic mixture of local anesthetics, Astra Pharmaceuticals, Sydney, Australia). The cream is a 1: 1 oil/water emulsion of a eutectic mixture of lidocaine (2.5%) and prilocaine (2.5%) bases.3 The eutectic mixture has a lower melting point (17°C) compared with the respective individual melting points of the lidocaine base (66-690C) and the prilocaine base (36-380C). This new physical property allows the lidocaine/prilocaine eutectic mixture to be liquid at mouth temperature and thus facilitate rapid absorption of the bases. It has become the treatment of choice when patients desire a needle-free method for topical anesthesia during venipuncture and IV catheter insertion17. However, effective analgesia requires the application of EMLA for 60 to 90 min, limiting its usefulness in busy ambulatory health care settings
References :
1 Asc G, Moore P, Needleman H, Shusterman S. The incidence of post extraction pain and analgesic use in children. Anesth Prog1986; 33: 147–151.
2 Primosch R, Antony S, Courts F. The efficacy of preoperativeanalgesia administration for postoperative pain management of pediatric dental patients. Anesth Pain Control Dent 1993; 3: 102–106.
3 Trijsburg RW, Jelicic M, van den Broek WW, et al. Exposureand participant modelling in a case of injection phobia. Psychother Psychosom 1996;65:57–61.
4 Hoffman PN, Abuknesha RA, Andrews NJ, et al. A model to,assess the infection potential of jet injectors used in mass immunisation. Vaccine 2001;19:4020–7.
5. Denne JR, Andrews KL, Lees DV, Mook W. A survey of patientpreference for insulin jet injectors versus needle and syringe. Diabetes Educ 1992;18:223–7.
6. Greenberg RS, Maxwell LG, Zahurak M, Yaster M. Preanesthetic medication of children with midazolam using the Biojector jet injector. Anesthesiology 1995;83:264–9.
7 Xavier B, Carraratti J, Orsola A, Garat JM, Vicenter GJ. [Topical anesthesia with EMLA cream: application in pediatric urology]. Actas Urol Esp. 1996;20:883–885
8. Serour F, Mandelberg A, Zabedda D, Mori J, Exra S. Efficacy of EMLA cream prior to dorsal penile nerve block for circumcision in children. Acta Anaesthesiol Scand. 1998;42:260–263
9. Halperin DL, Koren G, Attias D, Pelligrini E, Greenberg ML, Wyss M. Topical skin anesthesia for venous, subcutaneous drug reservoir and lumbar punctures in children. Pediatrics. 1989;84:281–284
10. Rylander E, Sjoberg I, Lillieborg S, Stockman O. Local anesthesia of the genital mucosa with a lidocaine/prilocaine cream (EMLA) for laser treatment of condyloma acuminata: a placebo-controlled study. Obstet Gynecol. 1990;75:302–306
11 Malamed SF. Sedation: A Guide to Patient Management. 4th ed. St. Louis, Mo: CV Mosby Co; 2003:199.
12. Kaufman E, Weinstein P, Milgrom P. Difficulties in achieving local anesthesia. J Am Dent Assoc 1984;108:205-208.
13. Ralph E, McDonland RE, Avery DR. Local anesthesia for the child and adolescent. In: McDonland RE, Avery DR, eds. Dentistry for the Child and Adolescent. 7th ed. St. Louis, Mo: CV Mosby Co; 1985:288-290.
14. Wright GZ, Starkey PE, Gardiner DE.Managingm Children’s Behavior in the Dental Office. St. Louis, Mo:CV MosbyCo; 1983:132-133.
15. Jorgensen NB, Hayden J Jr. Sedation: Local and General Anesthesia in Dentistry. 3rd ed. Philadelphia, Pa: Lea and Febiger; 1980:64.
16 Malamed SF. Handbook of LocalmAnesthesia. 5th ed. St. Louis, Mo: CV Mosby Co; 2004:274-275. |